Breast reconstruction: pros and cons
In what cases is breast reconstruction required
? ● If you think that reconstruction will give you a feeling of psychological comfort, “integrity”; ● Will help you regain a sense of femininity and confidence in your appearance; ● Restores symmetry if only one breast has undergone surgery; ● Allows you to wear low-cut clothing and open swimsuits.
Related procedures
If only one breast needs reconstruction, a breast lift, breast augmentation, or breast reduction may be recommended to achieve symmetry.
Advantages and disadvantages of breast reconstruction surgery
Pros:
● No need to use additional breast pads; ● Will relieve you of reminders about mastectomy and cancer; ● Will add confidence in your attractiveness and sexuality.
Minuses:
● Breast reconstruction involves surgery, medication, and additional costs; ● Breast reconstruction may interfere with the natural recovery of the body that has just undergone surgery; ● Reconstructed breasts do not have the same sensitivity as natural ones.
These are the three main pros and cons of breast reconstruction surgery. If you have individual questions, please consult with your plastic surgeon.
Breast reconstruction surgery: before and after photos
Is breast reconstruction surgery right for you?
Below are the main reasons why you should consider breast reconstruction surgery:
● The best results can be achieved if you are not overweight (body mass index below 30); ● You do not have circulation problems or other serious health problems such as high blood pressure or heart disease. Diabetes and autoimmune diseases - rheumatoid arthritis, scleroderma and others - increase the risk of infections or problems with wound healing. Bleeding disorders increase the risk of complications after flap surgery, and blood flow problems and anti-clot agents may increase postoperative bleeding; ● Smoking impairs blood circulation and can cause postoperative complications, delay recovery and lead to scar formation; ● Radiation therapy significantly influences the timing and method of breast reconstruction. It slows down wound healing and causes darkening and tightening of the skin. It is advisable to postpone breast reconstruction after radiation therapy for several months and use your own tissue transplant to replace the affected areas. ● Chemotherapy after a mastectomy may also affect the timing of breast reconstruction surgery. ● Previous surgeries, medical history and comorbidities are factors that will determine whether this surgery is right for you.
If you are in good health, have a positive attitude and have realistic expectations, this procedure is most likely safe for you.
About the operation
How is breast reconstruction surgery performed?
There are three main methods of breast reconstruction:
● Using implants (silicone or saline); ● Restoration using the patient’s skin, fatty tissue and muscles; ● A combination of the first two methods.
Basically, breast reconstruction techniques include several stages. Most procedures are performed on an outpatient basis, although some may require a stay in a hospital room (especially if performed in conjunction with a mastectomy). Implantation of an implant or expander will not take much time if it is performed immediately after a mastectomy. Your plastic surgeon will help you weigh the pros and cons to determine which method is best for you.
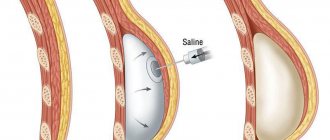
Reconstruction surgery using implants
As a rule, this process takes place in two or three stages. ● First, the surgeon implants a tissue expander under the skin and pectoral muscle, forming a skin-muscle cavity (capsule). A tissue expander is a saline implant with a valve that allows physiological saline to be added internally after surgery. A series of saline injections through the skin into the valve gradually fills the implant, increasing the volume of the breast. Visits to the doctor will take two to six months, during which time the skin-muscle cavity will stretch until you receive the desired implant size. ● Your next step will be an outpatient procedure during which the expander will be removed and replaced with a softer implant (saline or silicone). ● With saline implants, the expander is sometimes left in place for a longer period of time to reduce or increase the size of the reconstructed breast (by decreasing or increasing the amount of saline) without removing the implant. If a silicone implant is installed, the breast size can only be changed through another operation. ● In rare cases, the patient is given a saline or silicone implant without an expander. This is possible if, after a mastectomy, the size of the skin-muscle cavity is large enough to cover the implant.
Breast reconstruction with implants based on acellular dermal matrix Acellular dermal matrix (ADM) is skin tissue from which cells have been removed and a base of collagen and elastin is left for strength and elasticity. This tissue is prepared in a special way and allows the body's cells to grow into the material, completely replacing it with its own collagen and blood vessels.
During breast reconstruction:
● The acellular dermal matrix is a kind of “canopy” at the site of the postoperative dermal-muscular cavity. It supports the tissue expander and helps to better position the implant. This is the molecular basis by which the cells of the body grow into the matrix and, simultaneously with the expansion of tissues, regeneration occurs. Typically, the BMD is connected to the pectoral muscle to keep the expander and part of the implant from moving. ● The paper machine technique is less aggressive than the others. It allows you to create breasts of the required volume in a shorter period of time and reduces the number of visits to the doctor. With the use of BDM, it is possible to move from the expander to the final implant more quickly than with other tissue expansion techniques. In exceptional cases, you can do without an expander and place the implant in the cavity created during a mastectomy. In this case, no other operations are required. ● Using BDM, plastic surgeons have been able to offer emergency breast reconstruction to more patients, and the results after this operation have also improved. The quality of the chest cavity after mastectomy determines whether this technique is suitable for you or not. ● BDM has been used since 1994, and over the last ten years this technique has become very popular in breast reconstruction. PMs from different manufacturers have different properties, and depending on your condition, your plastic surgeon will advise which one to choose.
Natural grafts/flap grafting
In some cases, especially if you have had radiation therapy, your surgeon may recommend using a graft of your own skin to replace the damaged tissue with healthy, non-irradiated skin. ● Reconstruction using a flap of your own skin (autograft) looks more natural than breasts reconstructed with implants. However, this is a more invasive and complex procedure that usually requires hospital stay. In addition, scars remain on the body in the area where the flap was taken. ● Most often, skin from the back, abdomen or buttocks is used as a flap. In some cases, to restore the breast, it is necessary to transfer a section of skin along with muscle tissue, which makes this area of the body more vulnerable. ● Another way to treat tissue damaged by radiation therapy or small uneven areas is fat grafting. This procedure has its pros and cons, including graft loss and the formation of fatty tissue cysts. Multiple surgical procedures may also be required. After assessing your condition, your plastic surgeon will discuss the advantages and disadvantages of this surgery with you. Surgeons sometimes use fat grafting to improve results after implant restoration or to correct contour irregularities.
Skin sparing mastectomy
● If you are having breast reconstruction immediately after a mastectomy, your plastic surgeon may perform the procedure so that as much of the breast skin as possible remains intact. Along with the tumor and adjacent skin (free of cancer cells), the nipple, areola (pigmented skin around the nipple), fat and other breast tissue are removed. This preserves most of the skin on the chest. It can then be used to cover the flap or implant. ● The main advantage of this method of mastectomy is that for reconstruction it is not necessary to take skin from other parts of the body, which may not match the color, texture and thickness of the natural breast skin. ● For patients with large or sagging breasts, skin-sparing mastectomy is not recommended. Weakened skin can stretch even further and spoil the results of breast reconstruction surgery. If you are considering breast reconstruction, discuss this with your plastic surgeon before having a mastectomy.
Nipple sparing mastectomy
● This is a new technique in which the tumor and surrounding skin, fat and other breast tissue are removed, but the nipple and areola are left untouched. Reconstructed breasts look more natural. However, this method is not suitable for all women and can cause complications. In some cases, if the tissue is damaged, part or all of the nipple and areola will subsequently have to be removed. ● There is ongoing debate about whether retaining the nipple and areola will increase the risk of cancer coming back. It's best to discuss this with your surgeon, who can assess your risk based on your tumor type, family history, and other factors.
Nipple restoration using implantation
● The nipple and areola are restored after the permanent implant is placed in the operated cavity. This is the third stage. Re-creating the nipple and areola gives the new breast a more natural appearance and helps hide scars. ● The nipple is restored as follows: a flap of skin is lifted from the breast and folded so that a small protrusion is obtained. There are many ways to do this, and most of them are done in the office under local anesthesia. Many surgeons choose to delay nipple reconstruction until the implant is in its final shape, otherwise it may affect the position of the nipple in relation to the breast. ● An areola is usually created by tattooing the desired area or by grafting skin from the groin area. It is closest in tone to a natural areola. The transplant scar is hidden under the bikini line.
Which method should I choose?
The plastic surgeon will select a technique based on the individual characteristics of your breasts and your preferences. The main methods of breast reconstruction are discussed in the section “How is breast reconstruction surgery performed?”
Additional Information:
● After a mastectomy, there may not be enough tissue on the chest wall to cover and hold the breast implant in place. If the breast is being reconstructed after radiation therapy, a flap reconstruction will have to be done before using the expander. During this surgery, the surgeon grafts your muscle tissue, fat tissue, and skin to create a protruding breast. There are several methods of flap plastic surgery, the surgeon will select the most suitable one for you. ● Breast reconstruction after mastectomy using a tissue expander and implant is the most popular, since this procedure is performed quite quickly, on an outpatient basis. In exceptional cases, only an implant is used, without an expander. ● The surgeon will also give you a choice between a silicone and a saline implant. Silicone breasts are more similar in appearance and feel to natural breasts. However, both types of implants have their advantages and disadvantages, which your plastic surgeon will tell you about. One of the main advantages of a saline implant is that you will notice immediately if it ruptures - your breasts will decrease in size. In the case of a silicone implant, additional examination is required to confirm the rupture. ● Fat grafting is sometimes used to correct misshapen areas after lumpectomy and mastectomy. ● As a result of careful evaluation and selection of patients, nipple-sparing mastectomy and autologous breast reconstruction show good results. If you are suitable for this type of surgery, your surgeon will let you know.
What scars will remain after breast reconstruction surgery?
The following factors affect how the scars will look after full recovery: your age, genetics, your body's ability to regenerate, and the quality of the sutures. ● Even the best reconstruction cannot completely hide mastectomy scars. When breast reconstruction is performed in conjunction with a mastectomy, most of the skin on the breast is left to support the implant or flap of tissue. Then the mastectomy incisions can be hidden in the inframammary fold under the breast or in the areola area. Small scars on the areola are later painted over as a result of tattooing. ● After grafting with a flap, a long scar remains in the place where the skin was taken for grafting. Scars on the stomach or buttocks can be easily hidden under a swimsuit or underwear. In some cases, additional longitudinal or transverse incisions from the nipple are required for a more natural-looking breast. These scars become less noticeable over time, but never completely disappear. ● If a mastectomy is performed without reconstruction, the surgeon removes most of the breast using a large incision along the breast. In this case, the scar remains forever. If you subsequently have breast reconstruction, a second incision will be made in the same place to insert an implant or flap of skin. Thus, the scar remains on the reconstructed breast, but fades over time.
In order for the scar to resolve better, it needs to be moisturized, the scar line must be massaged, and special products will help soften it and make it less noticeable. As a last resort, if the scar does not resolve at all, the dead tissue is cut away and the incision heals again - this procedure can significantly reduce the size of the scar.
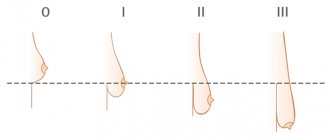
Indications for correction of nipples and areolas
Nipple correction surgery is in demand among both women and men. However, the indications for surgical correction of this part of the breast differ in male and female patients. The main reasons for turning to a plastic surgeon are the following conditions:
- asymmetry of the nipples: congenital or acquired as a result of plastic surgery, as well as arising due to age-related changes in the mammary glands;
- uneven contour of the nipple-areolar complex;
- thickened nipples;
- deformed areolas that have lost their round shape due to stretching;
- excess length of the nipple in women and an increase in the volume of the nipple-areolar complex in men;
- retracted nipple shape;
- large diameter of the breast areola;
- problems associated with breastfeeding, which are caused by the nipple being too small or large;
- trauma to the mammary glands, which led to deformation of the nipple-areolar complex;
- removal of mammary glands during treatment for breast cancer.
Nipple and areola surgery is an operation that allows patients to find psychological peace. Any aesthetic defects in the breasts in both men and women become the cause of serious complexes that negatively affect the patient’s self-esteem and quality of life.
Preparing for and performing breast reconstruction surgery?
Your plastic surgeon will give you any pre-surgery instructions, answer any questions you may have, take a medical history, and perform a physical examination to determine for sure whether the surgery will harm you.
Before your surgery, your surgeon will ask you to: ● Follow all preparatory instructions. As a rule, you need to do a blood test, fluorography and an electrocardiogram (ECG). ● To speed up the recovery process, you should not smoke for six weeks before surgery. ● Avoid aspirin and certain anti-inflammatory drugs and herbal remedies that may increase bleeding. ● Regardless of the type of surgery, hydration before and after is very important for a speedy recovery and good outcome.
Preparing your home for returning from the clinic To make your return home after surgery as smooth as possible, it is advisable to take care of many things in advance. ● Limiting heavy lifting after surgery is very important. If your breast has been reconstructed using flap surgery, then in most cases you should not lift anything heavier than 2 kg for 6 weeks. ● Prepare groceries ahead of time or have someone help you with your shopping. ● Do not vacuum, wash by hand, and avoid repetitive motions such as cleaning pots and pans.
Preparing for a comfortable recovery
Buy comfortable clothes in advance. ● You may not be able to put things on over your head. Prepare a comfortable jacket or jumper one size larger that fastens with buttons or a zipper. ● If abdominal muscle flap transplantation (TRAM technique) was used to reconstruct the breast, as well as for any micro-surgeries in the abdominal area, you need to buy loose pants so that the belt does not put pressure on the scar. Cotton pants one or two sizes larger will work well; you can pin them up with a pin and tuck the ends of the drainage into your pockets. ● You may find it awkward to bend over to put on your shoes. Bring some flip-flops, clogs, or mules. Take these clothes with you to the hospital or have someone bring them on the day you are discharged. Think about what car you will drive home. Bring pillows to support your back and neck, especially if the trip will take a long time. You can also use a pillow to support your stomach when you laugh, cough, sneeze, or fasten your seat belt.
Preparing the bed and bedside table before surgery
Most people are very nervous the night before surgery. If you put your house in order, distribute help with household chores and child care among friends and family, then you will be much calmer. The most important thing is to rest as much as possible after surgery. If you know in advance that everything will be taken care of for you, you will avoid unnecessary worries. ● You will need a lot of pillows for the bed, also place pillows under your back and legs to fix your hips and knees in one position. You may also want to place pillows under your arms. ● On your bedside table, within easy reach, place a small mirror, bacitracin or Aquaphor ointment, a phone (charger if needed), antibiotics, and pain medications. A TV remote control and a few good magazines or books would also help. ● Place measuring cups in the bathroom to drain the drainage, which your doctor will give you. Place a notepad with a pen nearby to write down the volume of fluid from the drain each time. ● You may need to see your doctor every week until all the drains are removed.
Breast reconstruction is usually performed on an outpatient basis. Agree in advance who can take you home after surgery and stay with you for at least the first night.
What should I expect on the day of breast reconstruction surgery?
Breast reconstruction surgery is performed in many clinics. As a rule, it lasts from two to six hours, in some cases longer. ● Medications are administered directly during surgery. ● Breast reconstruction surgery is usually performed under general anesthesia, but in some cases local anesthesia or intravenous sedation is preferable. ● For your safety during surgery, you will be connected to monitors to monitor your blood pressure, heart, pulse, and amount of oxygen in your blood. ● The surgeon performs the operation according to a plan that he discusses with you in advance. ● When the procedure is finished, you will be taken to the recovery room where you will be monitored for a while. ● Fatigue, thirst, and mild nausea may occur - these are side effects of anesthesia. You may be allowed to go home after a short rest period under medical supervision, unless your plastic surgeon intends to perform other post-operative procedures.
Cost of breast surgery
All measures related to the preliminary examination are included in the cost of correction of the nipple-areolar complex. If contraindications are identified that prevent plastic surgery, the patient pays only the cost of the examination. If there are no restrictions for the operation, then payment is made for the entire range of medical services performed, which may include subsequent rehabilitation with personal supervision by a plastic surgeon during the recovery process.
What is the price for nipple correction in Moscow? The cost of nipple-areolar complex plastic surgery depends on the type of surgery that the plastic surgeon will perform. Correction of a long nipple costs about 40-60 thousand rubles. The price of surgery for areola reduction starts at 15 thousand rubles. Complex surgical correction of nipples and areolas at the Maxim Osin plastic surgery clinic on an all-inclusive basis will cost patients 100 thousand rubles.
Recovery after surgery
The surgeon will tell you how long it will take to return to full activity and work. After surgery, you and your loved ones will receive detailed instructions about post-operative care, as well as: ● How to care for a drain (if you have one); ● Normal postoperative symptoms; ● Signs of complications.
Immediately after surgery
Your surgeon will tell you everything, but you can also expect the following:
● You may feel very thirsty and/or tired after surgery. ● Legs may be wrapped in compression bandages to improve blood circulation. ● Despite taking painkillers, you may still feel pain. ● To speed up your recovery, you may have drainage placed in your armpits (and abdomen, if an autotransplantation of a flap from the abdominal area was performed).
If plastic surgery with an autologous skin flap was used during breast reconstruction:
● A catheter will be inserted into your bladder and will be removed after surgery. ● The area where the flap for the new breast was transplanted may be painful. ● You may have difficulty getting out of bed without assistance.
If reconstruction was performed with a breast implant:
● The armpit area may be sore after surgery, but the arms and shoulders should be worked out. The surgeon will show you special exercises. ● The surgeon and nursing staff will help you get out of bed. The sooner this happens, the less likely it is that blood clots will form in the legs. ● You can perform water procedures yourself, but during the first week after some reconstruction techniques, outside help is desirable.
Think about who can pick you up from the clinic and stay with you during the first days of rehabilitation.
Pain may occur when the anesthesia wears off. If it is too strong and does not go away, consult your doctor. You may also experience redness and swelling after surgery. Ask your surgeon whether pain, redness, and swelling are normal symptoms or if they are signs of a complication.
Rehabilitation period after breast reconstruction
It is vital that you follow all of your surgeon's instructions. This information covers wearing compression garments, drainage care, taking prescribed antibiotics, and safe activity levels. The surgeon will also provide a detailed description of common postoperative symptoms and potential signs of complications. It is important to understand that the recovery period is individual for each patient.
Breast implants are the simplest and least painful method of breast reconstruction, and the rehabilitation period takes the shortest time. Typically, most women can resume normal activities within two to three weeks. Flap surgery is more complicated, since the operation is performed on two parts of the body, and the recovery period depends on the technique used.
In the clinic
After operations involving muscle tissue, it is necessary to spend some time in the clinic and limit activity. After TRAM flap surgery, you should not strain or lift anything heavy for six weeks. ● After surgery, you will be asked to move your arms, but not much. The staff will help you get out of bed or lie down. Most breast expander/implant reconstruction surgeries are performed on an outpatient basis, and you can be up and walking on the day of surgery. Walking helps blood circulation and prevents blood clots. ● How long you will stay in the clinic depends on your general condition, the type of surgery and the progress of your recovery. You may spend one to six nights in the hospital. After flap surgery, you need to stay in the hospital for 2-6 days, depending on the technique and the condition of the circulatory system. ● If the breast was reconstructed using a flap, a drain will be placed in the incision. If breast implants were used, the incision will simply be sutured or sealed with a special compound. ● The surgeon will recommend wearing an elastic bandage and a special bra to reduce swelling and provide additional support to the reconstructed breast. ● Before you go home, make sure you understand all the next steps for a speedy recovery. It's good if you have someone who can take care of you.
At home
● Depending on the type of surgery, you will have to spend a lot of time in bed or in a chair for the first few days. Many patients can walk without assistance on the second or third day after flap surgery. The surgeon will advise you to walk three to four times a day to increase blood circulation in your legs. ● You may find it difficult to shower in the first week, but if your surgeon allows it, you can do water procedures. You may need outside help. The ends of the drainage must be secured to a special belt with Velcro, and the clinic may also provide you with a bandage to secure the drainage around your neck. To make the procedure easier, try showering while sitting on a chair. You will get rid of this inconvenience when the drainage is removed. ● Ask for pain medications if needed. Without suffering from pain, you will recover much faster. ● At the beginning of the rehabilitation process, you will have to see the surgeon every week until the last drain is removed. Despite the inconvenience, there is no need to rush into this, as drainage helps the wound heal quickly. If less than 20-30 ml of fluid is released per day, the drainage can be removed. Typically, this is a painless procedure. ● Your new breasts may appear larger at first due to post-operative swelling. When it subsides, in a few weeks the breasts will take the desired shape. ● To speed up your recovery, you will be shown a set of exercises to perform at home. At first, you may experience discomfort when moving your arms. It is important not to stop and continue doing the exercises. ● How soon you can return to work depends on your occupation and type of surgery. If you are not doing hard manual labor, you will soon be allowed to work. Remember that you may experience increased fatigue at first. ● If you are no longer taking painkillers, you can drive. In case of an emergency stop or a sharp turn, you need to control the handbrake well and shift the gearbox, and taking painkillers significantly reduces the reaction. ● As the wound heals, itching may occur, but do not scratch the area. The itching will gradually subside. Usually the wounds heal completely within six weeks and the itching disappears. Remember that this process involves several stages, and the inflammation phase can last several months (in this case, the edges of the wound are pink or purple in color and protrude slightly above the surface of the skin). After a year, the scars will become less noticeable. Be patient and follow the surgeon's recommendations to help the scars resolve better.
How long will the results last?
When reconstructing with breast implants, you can be confident that both saline and silicone implants are safe and effective when properly cared for. Manufacturers provide a lifetime warranty on all types of implants, but the longer you use them, the greater the risk of complications. According to recent data, 95% of implants remain intact after seven years. However, according to other data, half of women who reconstructed their breasts with implants replace or remove them ten years after the operation. ● For those patients who have had one breast reconstructed, the differences between natural and artificial breasts will become noticeable over time. Natural breast tissue is prone to wrinkles and loss of elasticity, unlike an implant, which keeps the breasts young and prevents them from sagging over time. ● In patients who have undergone a double mastectomy and double breast reconstruction with implants, the breasts retain their shape and youthful appearance without wrinkles even at 70 years of age. ● Breasts reconstructed with a flap are subject to the same gravitational forces as natural breasts. Tissue may age differently because it was transplanted from other areas of the body. ● Skin and fat tissue from the upper back or buttocks are thicker and more elastic, so they age and sag more slowly than breast tissue. ● The structure of the skin and fatty tissues of the abdomen coincides with the skin of the breast, so such breasts also sag and age over time, like natural breasts.
Maintaining a Relationship with Your Plastic Surgeon
For safety and best results, it is important to see your plastic surgeon after surgery, especially if you notice any changes. Don't hesitate to contact your surgeon if you have any questions or concerns.
Possible complications after breast reconstruction
Fortunately, serious complications after breast reconstruction are rare. The surgeon will discuss possible risks for you at your preliminary consultation.
All surgical procedures carry some risk. Potential complications that apply to all operations: ● Negative reaction to anesthesia; ● Hematoma or seroma (collection of blood or fluid under the skin that may require removal); ● Infection and bleeding; ● Changes in skin sensitivity; ● Scar formation; ● Allergic reactions; ● Damage to the lower layers of skin; ● Unsatisfactory results, which may require additional procedures.
Specific risks of breast reconstruction surgery: ● Formation of necrosis or fatty tissue cysts; ● Formation of blood clots in the legs or lungs; ● Partial or complete loss of a flap of skin; ● Loss of sensation in both the donor and reconstructed areas.
Complications at the donor site of the body: ● Hernia; ● Slow wound healing, poor scar formation; ● Breast hardening (capsular contracture); ● Implant displacement; ● Implant rupture.
Following your plastic surgeon's advice and instructions before and after breast reconstruction surgery will help you significantly reduce your risk of complications.
Lyn Dunham
Another star to join the Free the Sipple movement is the Girls actress. In 2020, Lena Dunham published a topless photo with her nipples covered with a scarf.
It is not surprising that she supports this direction, because from the very beginning of her career she had no problems showing off her figure, and she often shared nude and provocative photos. According to her, she feels as confident without clothes as she does with them on.
6