How is a mastectomy performed?
The appearance of mastectomy scars depends on the type of surgery that was performed.
Often, the appearance of the scars left after a mastectomy depends on the incision and the technique the surgeon uses.
At the beginning of the operation, the surgeon will make an incision in the skin of the chest to expose the inside of the breast.
Once the surgeon has removed the breast tissue, as well as the muscle and, if necessary, lymph nodes, he will immediately sew up the skin where the incision was made.
When the tissue damage heals, scars will appear on the skin of the chest. Despite the various surgical approaches described in the current material, most mastectomy scars form a horizontal line across the chest, and sometimes these scars have a crescent-shaped appearance. Quite often, the type of incision the surgeon makes and the resulting scars depend on where the cancer first affected the mammary glands.
Over the decades, the techniques used by surgeons during breast surgery have undergone significant changes. Currently, there are a large number of different procedures that are becoming more accessible to women every year. Of course, before surgery, the patient should ask her surgeon what surgical method he intends to use and what results can be expected.
Consequences of mastectomy
This operation is one of the complex surgical interventions. It is performed over several hours under general anesthesia. Therefore, recovery takes a long time. After a mastectomy, the patient develops an extensive wound field that requires competent care. Of course, this operation does not always go without complications.
Experts highlight:
- Early and late postoperative complications.
- The occurrence of relapses of a malignant disease.
- Serious psychological stress associated with loss of attractiveness and disability.
Everyone knows that forewarned is forearmed. A woman undergoing a mastectomy should be aware of the possible consequences of the operation and how to overcome them.
Early complications
In the early period after mastectomy, the following types of complications are distinguished:
- Bleeding. They occur for several reasons: poor blood clotting, sutures coming apart, a blood vessel not being sutured. Bandaging is used to stop bleeding; in case of poor clotting, medications are prescribed. If the cause of bleeding is an oozing vessel, then a repeat operation is performed.
- Lymphatic drainage is often found during mastectomy, because lymphatic vessels are excised and removed along with the mammary gland. To overcome the consequences of surgery, drains are installed in the wound. In case of severe lymphatic leakage, a puncture is performed.
- Infection of a wound can occur for various reasons: violation of the rules of asepsis (measures to prevent infections) during surgery or during the dressing process; the source of infection can be the patient’s skin. To prevent infection of the surgical site, a course of antibiotic therapy is prescribed before and after surgery.
Late consequences
In a longer period, a patient who has undergone a mastectomy may experience:
- Lymphedema after mastectomy of the upper limb. After surgery, the lymphatic system does not recover for a long time, the outflow of lymph is difficult. Many patients experience swelling after shoulder mastectomy, they feel pain in this area and limited mobility. Sometimes the arm after a mastectomy begins to lack nutrients, this leads to serious trophic disorders and the occurrence of lymphostasis (giant limb). This disease is very difficult to treat; restoration of the mammary gland is almost impossible. To prevent lymphostasis, the patient is prescribed courses of vitamins to restore trophism and a hand massage after mastectomy to normalize lymph outflow.
- Erysipelas. Another type of complications associated with disturbances in the outflow of lymphatic fluid. A certain type of streptococcus enters tissues with impaired trophism, which provokes the development of an infectious process. The patient's temperature rises, headache, chills, nausea appear, and redness and swelling of the limb develop. Erysipelas is treated with antibiotics. It is important to start taking them at the very beginning of the disease, otherwise there is a risk of an abscess or bleeding.
- Formation of keloid scars after breast removal. Rough scars may appear at the site of the sutures due to disruption of tissue trophism. They cause pain when moving and impede the drainage of lymph. They are removed by excision.
- Restricted mobility of the shoulder joint, loss of skin sensitivity. As a rule, intensive treatment and massage help restore joint mobility and sensitivity of the shoulder skin.
- Phantom pain. Some patients complain of periodic pain at the site of breast removal. In this case, they are prescribed a course of sedatives and medical massage.
A quick recovery after a mastectomy depends not only on the doctor, but also on the patient herself.
What types of mastectomies result in scars?
Any type of mastectomy results in scars of varying severity. However, there are a number of approaches that a surgeon can use.
Partial mastectomy or lumpectomy
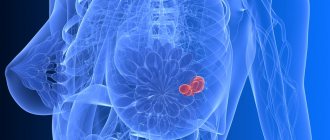
A partial mastectomy involves removing the tumor and some area of breast tissue. Sometimes the surgeon also removes the layer of tissue that covers the chest muscles.
A lumpectomy usually leaves a straight scar on the skin of the chest. Sometimes the surgeon may be able to make an incision in the crease of the breast or around the nipple to try to hide the scar.
A partial mastectomy usually leaves most of the breast intact, so breast reconstruction is usually not required. Women who have had a lumpectomy often need follow-up radiation therapy.
Skin sparing mastectomy
This surgical method is usually performed if a woman intends to undergo breast reconstruction immediately after undergoing the main procedure. A skin-sparing mastectomy involves removing the breast, areola, nipple, and lymph node or nodes. But at the same time, the surgeon leaves the breast skin.
Preserving most of the breast skin allows for immediate reconstruction using either implants or the woman's own tissue. Skin-sparing mastectomy usually leaves a visible, medium to large scar on the front of the breast. However, the surgeon can hide this scar by making an incision in a less obvious location.
Nipple sparing mastectomy
Women who undergo prophylactic or precautionary mastectomy, as well as those who have early stage breast cancer, may be candidates for nipple-sparing mastectomy (nipple-sparing mastectomy). This procedure also involves preserving the skin of the breast and areola.
This surgical approach is usually offered to women with small breasts and leaves a scar on the side of the breast. However, the surgeon can also make an incision in the breast crease, that is, on the bra line, and thus make the scar invisible.
Simple mastectomy
This type of surgical approach involves removing the breast, areola and nipple, and sometimes lymph nodes and some area of breast skin, the area of which depends on the woman's plans for reconstruction. The chest wall and lymph nodes located distant from the operated breast, for example, in the axillary region, are preserved.
Typically, the surgeon makes an oval-shaped incision that goes around the nipple across the entire width of the breast. This incision leaves behind a significant and visible scar.
Modified radical mastectomy
This method involves the surgeon removing all of the breast tissue, as well as the lymphatic vessels in the chest and armpit area. The chest wall usually remains intact. A modified radical mastectomy leaves a large, visible scar on the chest.
What additional treatment is required after a mastectomy?
The main goal of a mastectomy or any other cancer surgery is to remove the minimum amount of tissue necessary to treat the cancer.
Causes
Many women know that after breast surgery, for example, after a lumpectomy or mastectomy , scars will certainly form. But few people know that other breast cancer treatments can also lead to scarring.
For example:
- Surgical drains placed in your breasts after surgery will leave small, round scars when removed. The amount of scarring will depend on how many drains were installed and how long they were in place.
- The chemotherapy port system (in addition to administering cytostatic drugs, the medical device can also be used to draw blood) leaves a scar at the incision site (just above the chest near the collarbone).
- Radiation therapy can cause fibrosis , i.e. excessive growth of fibrous connective tissue, which leads to uneven thickening of the skin. Even short-term effects of radiation therapy, such as skin irritation and blistering after a burn, can leave permanent marks. It is also common for radiation therapy to leave a permanent “tan” in the chest area.
- Scars remain after surgery to remove lymph nodes.
How is breast reconstruction performed after a mastectomy?
Reconstruction is a surgical procedure performed after a mastectomy to improve the appearance of one or both breasts. It can be performed either at the same time as a mastectomy, or after a certain period of time.
To perform the reconstruction, the surgeon may take tissue from another area of the woman's body, use implants, or use a combination method.
Tissue expansion and implants
If a woman decides to reconstruct her breasts with implants, the doctor will need to place a device called a tissue expander under the chest muscles or under the skin of the breast.
This procedure can also be performed either at the time of the mastectomy (immediate reconstruction) or later (delayed reconstruction). The woman will need to visit the doctor several times to fill the implant with a saline solution for expansion.
Once the chest skin has stretched and healed from surgery, the surgeon can prepare permanent implants. This time usually occurs approximately 2-6 months after the mastectomy.
However, some women receive permanent implants directly during a mastectomy.
Reconstruction using autologous tissue
Another popular method of breast reconstruction is reconstruction using autologous or own tissue. During this procedure, the doctor takes tissue from the woman's abdomen, back, or buttocks and uses it for reconstruction along with the area of breast skin that was saved during the mastectomy.
This type of procedure is more complex because the surgeon sometimes has to restore blood circulation to the breast tissue.
This type of reconstruction can also be performed either directly during the mastectomy or after some time.
Prevention of postoperative edema
After breast removal, regardless of the type of operation, measures are taken to prevent the development of edema. This is due to the fact that the incisions are accompanied by damage to the lymphatic vessels and impaired lymph outflow. Intercellular fluid accumulates in the area of the postoperative wound, which slows down tissue regeneration and also creates favorable conditions for the development of infection. After mastectomy with removal of regional lymph nodes, the severity of congestion increases. The fight against edema includes several measures:
- A post-mastectomy bandage to be worn after surgery. The product compresses the tissues of the postoperative wound area and helps prevent their swelling.
- Compression underwear - a tight-fitting T-shirt, a special bra - promote moderate tissue compression to prevent swelling. Special postoperative underwear should be made of cotton fabric. Synthetics contribute to the development of complications, as they do not allow the skin to “breathe”, provoke the addition of a bacterial infection, and worsen blood circulation in the tissues. Any clothing should not have tight elastic bands.
A balanced diet with sufficient protein intake promotes rapid wound healing. At the same time, the skin will itch.
To prevent the formation of a keloid scar, you should not sunbathe, as the ultraviolet spectrum of sunlight causes the wound to heal poorly. In the future, the area of the operation may be determined in contrast against the background of a tan.
What if a woman does not want breast reconstruction?
Although breast reconstruction after mastectomy is very popular, some women refuse this procedure
According to BreastCancer.org, about 44% of women who undergo mastectomy do not express a desire for further reconstruction.
Women choose not to undergo reconstruction for a number of different reasons. This series includes:
- health problems that may make future surgery unsafe or unwise;
- the desire to quickly restore normal daily activity;
- fear of using tissue from other parts of your body or implants during reconstruction;
- high cost of reconstruction.
Sometimes women who do not want to have their breasts reconstructed decide to use prosthetics (artificial breasts), which can be placed in a bra. These women also have access to a sticky pear-shaped device that is attached to the body.
Many women do not use either reconstruction or prostheses and refuse to explain their decision.
After breast removal: how to get back what was lost?
Breast defects are a “sick” topic for women, which they perceive as a real life tragedy. But even in the most difficult cases, which primarily include mastectomy, plastic surgeons can help. In Novosibirsk, the Siberian Institute of Beauty, headed by Professor Olga Borisovna Dobryakova, has been restoring mammary glands and correcting congenital defects for many years.
Women after mastectomy: what next?
Breast cancer ranks first among all cancers in women. Detected in a timely manner, it is now quite successfully treated, but the price of such treatment is most often breast loss. In our country, mastectomy - surgical removal of the mammary gland - is the main method of treating malignant tumors. Moreover, as a rule, surgeons act radically: the gland is completely removed.
So, having defeated cancer, women are faced with another problem that causes them no less torment: how to live with such an aesthetic defect?
Plastic surgeons come to the rescue. They can reconstruct the removed mammary gland, achieving a good visual effect. During the operation, it is possible not only to restore the natural volume, but also to improve the shape of the breast in accordance with all aesthetic canons.
“We perform reconstructive mammoplasty not only after cancer. There are other diagnoses that require aesthetic correction. Underdevelopment of the mammary gland, defects after injuries, pronounced asymmetry of the mammary glands; reconstruction of the mammary glands in transsexuals can be placed in the same category.”
, says Olga Dobryakova, professor, doctor of medical sciences, plastic surgeon, director of the Siberian Institute of Beauty.
All types of plastic surgery are performed at the Siberian Institute of Beauty. Olga Borisovna has performed hundreds of operations to correct defects of the mammary glands. She devoted several hundred scientific articles and textbooks to this topic. The clinic has its own developments, proprietary techniques for performing surgical interventions, which make it possible to recreate the breasts as natural and harmonious as possible.
Breast reconstruction: how shape and volume are created
There are several methods for breast reconstruction. Often, for this purpose, one’s own tissues (autologous tissues) are used - flaps that are transported from different parts of the body. The most common use of the TRAM flap is the transverse rectus abdominis muscle flap. In addition to this, there are flaps from the latissimus dorsi muscle, buttocks, and the lateral surface of the torso. The flaps can be “non-free”, that is, transplanted together with a feeding “pedicle”. Or “free” flaps that are transplanted, and microsurgical work to connect blood vessels takes place in a new place.
Based on my experience, I can say that the visual effect of reconstructing the mammary gland using muscle flaps is good.
Over time, a gradual slight decrease in the gland may occur due to atrophy of muscles and subcutaneous fat, but we initially prevent this by creating a flap that is slightly larger in volume. Olga Dobryakova
The second method is expander dermotension. In the area of the removed mammary gland, tissue deficiency inevitably occurs. In order to restore volume to the breasts, the tissue must first be stretched. This can be done using an expander. This is a “balloon” that is placed in the desired area and is gradually filled with a solution, gently stretching the tissue.
There are several types of expanders. They may differ in type of material and service life. Silicone expanders, according to experts, have good durability, so they are preferable to latex ones, which carry risks of leakage.
In addition, expanders can be permanent or temporary. “Prosthetic expanders” are installed once and do not require replacement with an implant - they are initially filled with silicone gel, the volume of which is replenished by saline solution introduced in stages. A temporary expander is used only to stretch the tissue, and after that it is replaced with a silicone endoprosthesis.
With the help of expander dermodesia, you can achieve the desired volume, beautiful shape, and naturalness of the mammary glands. However, this is not always easy. If you plan the operation incorrectly, you can get the effect of a bump, which will look very unaesthetic on the body. In particular, this happens when the doctor opts for a small expander and is in too much of a hurry to complete the work.
“How to get the desired result? I take a large expander and stretch the tissue very slowly over a long period of time. It may take six months or a year for a mammary gland to form with a clear submammary fold. This is the only way the breasts will end up looking like real ones.”
, - Dobryakova shares his professional secrets.
The author's developments include the introduction of botulinum toxin before stretching. Reacting to the injections, the tissues relax and stretching occurs more effectively.
Patient, slow stretching of tissues using an expander can increase their volume tens of times. This allows the surgeon to form a mammary gland that is as close to natural as possible.
Sometimes breast reconstruction requires a combination of both methods - placing a flap and then stretching the tissue with an expander. For example, if a patient has ulcerative defects, they must first be covered with a flap, and then work on the volume.
The second gland may also require correction. If it is irregularly shaped, or has severe ptosis, it also needs to be brought into shape, sometimes with the help of an implant. This is how the doctor achieves symmetry of the mammary glands and recreates the overall aesthetics of the female breast.
The artistic element is very important in reconstructive mammoplasty. Just “making breasts” is not difficult. And making natural breasts is a creative process that requires effort and special skills of a plastic surgeon.
Nipple-areolar complex: methods of restoration
After the volume and shape of the gland has been created, it is necessary to reconstruct the nipple-areolar complex. There are several ways to restore it.
To recreate the areola, today a technique is used to transplant pigmented skin from different areas of the body: from the inner surface of the upper thigh, labia. If possible, the second areola can also become a “donor”. Plastic surgeons identify these methods as the main ones, and alternative methods include creating an areola using a tattoo, for example.
“Skin grafting taken from the upper part of the inner thigh gives a good aesthetic effect and the healing of such flaps usually occurs without problems. In addition, this method can be considered the most reliable and psychologically comfortable for patients.”
,” Olga Borisovna shares her observations.
After recreating the areola, surgeons are faced with another task - it is necessary to form a nipple on it. Various techniques are also used for this. For example, there are known methods for cutting out the nipple protrusion using flaps in the center of the areola.
At the Siberian Institute of Beauty, the author’s technique, developed in 2010 by professors O.B., is used to recreate the nipple. Dobryakova, B.S. Dobryakov. It consists of using an implant – a silicone ball.
The Siberian Institute of Beauty has more than a dozen inventions that have opened up new possibilities for aesthetic surgery. Reconstructing the nipple using a silicone ball is an original technique that has improved the results of reconstructive mammoplasty.
At the first stage, a silicone ball is inserted into the donor site, which is most often located in the upper part of the inner thigh. Within 1-2 months it remains under the skin, growing into a strong connective tissue capsule. It is then removed and placed in the center of the areola, forming the nipple.
The goal of reconstructive mammoplasty is to make the breasts look beautiful and natural. Moreover, not only in underwear, but also without it. If a woman who has undergone surgery (and sometimes more than one) still cannot afford to undress, it means that the reconstruction was pointless, and time, money and nerves were wasted.
“I consider such breast reconstructions to be a special merit when, after restoration, the mammary glands become so natural and harmonious that they look even better than before the oncological operation.”
, says Professor Dobryakova.
“I have never had such beautiful breasts as now, I feel not just a full-fledged person, but also a desirable woman, I am happier than ever,” this patient’s review is the highest assessment of my work.
Olga Dobryakova
Siberian Beauty Institute:
2-910-946, outpatient clinic: Novosibirsk, st. Novaya Zarya, 17 A; hospital: Novosibirsk, st. Zalesskogo, 6, building 9, 7th floor, room. 737; www.dobryakova.ru
https://m.vk.com/olga.dobryakova
https://www.imgrum.org/user/sib.institutkrasoty/3283685133
https://www.instagram.com/sib.institutkrasoty/
There are contraindications. Specialist consultation is required.
How to improve the condition of sutures after mastectomy without reconstruction?
If a woman decides not to undergo reconstruction, she should talk with her doctor about surgical options that can maximize the improvement of the scars left in the skin after a mastectomy.
For example, the surgeon may take steps to make the sutures flatter against the surface of the skin, resulting in a smoother chest wall. Otherwise, a woman may be left with rough scars on her chest, which creates a lumpy appearance of this area of the body.
Even though it does not cause any physical discomfort, women do not like the look of such scars.
Sometimes the surgeon may make what is called a Y-cut, that is, make two small incisions as additions to the main one. This technique can slightly reduce the protrusion of the skin.
Tattoos after mastectomy
In February 2020, the Journal of the American Medical Association published an article, “The Healing Role of Tattoos After Mastectomy.” The story revealed details of the work of a tattoo artist who often has to apply designs over mastectomy scars.
This is a new approach for women who decide not to have breast reconstruction.
Some women who have undergone breast reconstruction go to tattoo parlors to get nipple tattoos. These tattoos give the nipples an additional three-dimensional effect. There are masters who specialize in working in this direction.