When a person develops a myocardial infarction, blood flow in one or more coronary vessels is disrupted. This leads to an imbalance between the need of myocardiocytes for oxygen and its supply. Changes in metabolism due to lack of nutrients aggravate the condition of the affected tissue. As a result, cardiac muscle cells begin to necrotize and die. In place of the dead tissue, a scar forms. In this article I want to talk about the mechanism and possible consequences of such a “replacement”.
Development mechanism
At the time of the development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Stages of healing
The process of tissue restoration consists of the following stages:
- During the first 24 hours after surgery, a blood clot forms in the socket. The formation closes the wound and protects against infection and food debris. Subsequently, the clot takes part in healing, so specialists urge not to touch or rinse the wound for the first day;
- After 3-4 days, the wound becomes covered with a white film, which indicates the formation of epithelial cells. The wound may have a yellow or grayish tint due to food pigments. If the wound is green, dark, or there is a putrid taste in the mouth, then you should visit a doctor;
- After 7-10 days, the gums become covered with a white coating, under which young granulation tissue is formed;
- On days 18-25, the wound heals and heals;
- Next, bone formation occurs, which can last 4-6 months.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Symptoms of the recovery period
Following the doctor’s recommendations speeds up the healing of the hole after tooth extraction and minimizes the risk of complications. However, for 3-5 days the patient may experience the following symptoms:
- increase in body temperature to 37.7-38.5 degrees;
- pain in the area of the postoperative wound;
- slight bleeding from the socket.
These symptoms do not indicate the development of complications; they are characteristic of the normal dynamics of regenerative processes. The next section of the publication will tell you when it’s time to sound the alarm.
We suggest you familiarize yourself with Thrush on the lips in children
Classification
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can be observed from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
Diet
Making healthy food choices helps the healing process.
Recovering from heart surgery requires focusing on a healthy diet. This will help the body heal, reduce the risk of complications and enable the patient to recover faster. Many studies have shown that a diet rich in fruits, vegetables, nuts and seeds can reduce the risk of heart disease.
Appetite may decrease noticeably, and food may lose its usual taste. The patient may also experience a strange metallic taste in the mouth. This is usually caused by surgery or related to medications. Full recovery may take 3 months. It is recommended to eat small portions frequently.
A healthy diet provides the body with many nutrients - such as vitamins, minerals, antioxidants and dietary fiber.
The diet should include:
- Meat and/or meat alternatives such as eggs, tofu, legumes and nuts;
- Fish – 2 buttery fish meals per week, such as salmon, mackerel or sardines, will help you get plenty of healthy omega-3 fatty acids;
- Wholemeal bread or crackers, brown rice, wholemeal pasta, quinoa, barley, rye, couscous;
- Dairy products - preferably low fat;
- Healthy fats – small amounts of healthy fats and oils from nuts, seeds, avocados and fatty fish;
- Water – Avoid sugary soft drinks and alcohol.
The goal is to consume 2 meals of fruit, 5 meals of vegetables, and 4 or more meals of whole grains - depending on your energy needs.
More tips to help you eat well:
- Reduce salt intake - use as little salt as possible when cooking as this will help lower blood pressure and help prevent fluid retention;
- Avoid sugary foods - they are often eaten as a substitute for healthy foods and can contribute to weight gain.
If your appetite does not return within a few weeks, you should tell your doctor.
Emotional condition
It is common for patients to feel sad or depressed after heart surgery, but these feelings should subside after the first few weeks.
To improve your mood:
- Walk daily;
- Devote time to hobbies and social activities;
- Talk openly about your feelings to loved ones;
- Sleep well.
Sex after surgery
In the first two weeks after heart surgery, most people are at high risk of heart problems during sex as a result of increased heart rate and blood pressure. However, this risk becomes significantly less by six weeks after surgery.
While recovering from heart surgery, you may experience intermittent chest pain, abnormal heart rhythms (arrhythmias), or heart failure, which increase your risk of heart problems during sex. People in these risk groups need additional assessment/or treatment before attempting sex.
The doctor will assess the patient's condition and advise when it is safe to resume intimate relationships.
Sexual problems
The patient may experience decreased sexual activity and desire. Various factors may contribute, including medication side effects, depression, and concerns about triggering another heart attack or death. You should not worry about decreased sexual interest; after the body is fully restored, your previous sex life will return.
Physical exercise
Since it takes 6-8 weeks for the breast bone to heal after heart surgery, you should slowly return to your normal activities.
When can you resume daily activities:
- Driving. Do not drive for 4-6 weeks unless advised by your doctor as concentration, reflex time and vision are often affected within 6 weeks.
- Sex. Sex requires about the same amount of energy as walking up two flights of stairs, as a rule, the patient is ready to return to this from about the 3rd week (loss of interest in sexual activity for a while is normal, however, the patient should return to normal life in 3 months).
- Job. The patient can return to work as soon as concentration, confidence and physical ability allow. Typically, returning to an office job (or any other job without physical and psychological stress) is possible after 3 months, to a job involving hard work - after six months.
- Housework. You should start with the things that the patient likes to do most and which are easy for him: cooking, caring for flowers, cleaning, scrubbing, washing. Heavier work is not recommended.
How dangerous is this?
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
What causes scarring on the heart muscle?
What is a heart scar? In fact, it is connective tissue that fills the space created as a result of damage to a certain area of the heart muscle. This happens with an inflammatory disease or myocardial infarction, which is caused by various factors. The appearance of numerous notches on the heart can occur due to progressive vascular atherosclerosis.
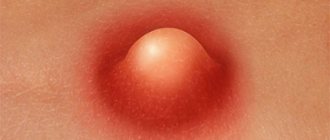
The appearance of scars is caused by the death of heart cells as a result of blocking the access of oxygen-enriched blood to them. A common cause of heart scars is thrombosis. If a person has a prolonged vascular spasm, this will lead to partial necrosis of the organ. Other diseases that cause scarring of the heart include:
- Cardiac form of rheumatism. With this type of disease, inflammation of the myocardium and cardiac membranes occurs. As a rule, the pathology is a consequence of frequently recurring tonsillitis, chronic tonsillitis, scarlet fever and streptococcal diseases. In this case, damage to the epicardium is observed, which ultimately ends in scarring and thickening, which is necessary to restore and maintain the functionality of the heart.
- Myocarditis. If a person has previously suffered any infectious diseases that resulted in complications in the form of inflammation of the heart tissue, this can cause scarring. Intoxication as a result of poisoning and parasitic infestations also leads to this.
- Cardiac ischemia. This pathology accounts for 90% of all deaths from heart disease. It is the cause of numerous scars, and can also be a consequence of their appearance. This creates a vicious circle that quickly leads the patient to a heart attack or stroke.
- Myocardial infarction. In most cases, a heart attack ends in death, but if the patient received timely medical care and survived as a result of resuscitation measures, scarring will occur. This condition is the main cause of the proliferation of connective tissue, which fills the wound formed after cell necrosis.
The cause of scars can be not only the presence of one or more diseases of the cardiovascular system, but also an incorrect lifestyle, endocrine disorders, and severe stress.
The development of cardiosclerosis can be indirectly affected by the following pathological conditions:
- diabetes;
- anemia;
- obesity;
- amyloidosis;
- metabolic disease;
- premature wear of the heart as a result of heavy physical exertion;
- hemosiderosis.
In rare cases, cardiosclerosis can be detected in a child with congenital heart defects. Some adults experience a mild heart attack on their legs, thinking they are having an attack of tachycardia or angina. Sometimes a person suffering from a suffocating cough turns to a therapist for help, and the therapist, having not found the reasons for its occurrence, sends the patient for a comprehensive examination. As a result of EGC or ultrasound, cardiosclerosis is detected. In this case, the patient needs to make an appointment with a cardiologist, find out the main reason for the appearance of scars on the heart and begin treatment.
Complications and their symptoms
All complications are associated with inflammation and the development of infection at the site of the extracted tooth. The most common complication is alveolitis - inflammation of the bone socket after tooth extraction. Periostitis, an inflammation of the periosteum of the jaw bone, may also develop. Less commonly, a cyst develops at the site of an extracted tooth.
Only a specialist can diagnose the complication. The patient’s task is to suspect the development of a pathological process in a timely manner and promptly seek medical help. You should remain alert for the following symptoms:
- Hyperemia and severe swelling of the gums.
- Repeated heavy bleeding.
- Exacerbation of pain syndrome.
- Temperature rise above 38.5 degrees or 5 days after extraction.
- The appearance of purulent discharge from the wound.
- Swelling of the cheek on the side of the operation.
- Bad breath.
If one or more symptoms of a complication appear, you should contact the doctor who performed the extraction. Delay is fraught with the development of a pathological process with spread to bone tissue. This can lead to osteomyelitis, which is difficult to treat.
What is the danger?
If a person develops a scar on their heart after a heart attack, it can lead to coronary artery disease, heart failure, and an aneurysm. Much depends on what type of disease the patient suffers from. Cardiosclerosis is divided into:
- Diffuse. With this type of disease, a uniform thickening of the walls of the heart muscle occurs due to the appearance of pinpoint foci of connective tissue on them. In this case, large scars may not occur.
- Large-focal. The most dangerous type of cardiosclerosis, since it involves the replacement of large affected areas with fibrous tissue that is unable to contract. As a result of dysfunction of the cardiovascular system, serious diseases begin to develop, most often ending in death.
- Finely focal. This type of disease has a generally positive prognosis with proper treatment and systematic testing. This form is the result of a microinfarction, after which one small scar remains on the heart, which does not significantly limit the functionality of the organ.
Sometimes the appearance of a scar on the heart goes away almost unnoticed and the person continues to live without taking any measures. But it is possible to detect cardiosclerosis without undergoing special diagnostic procedures, based on the characteristic symptoms of the disease:
- cardiopalmus;
- dyspnea;
- fast fatiguability;
- constantly cold hands or feet, as well as their numbness;
- swelling of the face;
- exercise intolerance;
- blueness of fingertips.
A person who has scars on the heart suffers from severe chest pain, which can be paroxysmal (paroxysmal) in nature, looks pale due to insufficient blood supply to the tissues as a result of cardiac dysfunction.
The main consequences of cardiosclerosis are atrial fibrillation, extrasystole, heart block, stroke and heart attack. These are serious diseases that most often cause disability and death.
Surgical care for scars
Surgery is indicated only in emergency situations, when the patient is in critical condition and drug therapy is powerless. The following types of operations are carried out:
- Shunting. It consists in expanding the lumen of the coronary vessels.
- Heart transplant. Performed on patients under 65 years of age.
- Removal of the aneurysm. Under general anesthesia, a protruded area of one of the walls of the left or right ventricle is excised.
The scar after surgery heals quite quickly and rarely causes severe discomfort to the patient. After the rehabilitation period, the patient can return to a normal lifestyle, but with mandatory adherence to a special diet and further drug therapy.
A scar on the heart in medical terminology is called cardiosclerosis. The essence of the pathological process is the death of cardiac muscle cells and their replacement with connective tissue, this can happen after a heart attack or as a result of an inflammatory process. An ECG helps identify changes in the heart muscle and specify the extent of damage.
This process is dangerous for the patient’s life, since fibrous tissue is tougher in structure than muscle fibers; it is not able to contract in a rhythm synchronous with all other parts of the heart. For patients experiencing heart scarring, it is important to know the causes of this phenomenon and to prevent further changes in the heart muscle. Without appropriate help, the consequences of fibrosis can be very diverse, from heart failure and aneurysm of the lower wall of the heart to sudden death as a result of a second heart attack.
How recovery rates depend on indications for extraction
It is impossible to give a universal answer to the question of how long it takes for gums to heal after tooth extraction. The rate of regeneration directly depends on the characteristics of the clinical case, that is, on the indications for extraction. In surgical dentistry, there are several direct indications for the removal of defective or diseased elements:
- Chronic periodontal disease with pathological mobility of teeth 3 degrees.
- Acute purulent periodontitis or exacerbation of chronic periodontitis with localization of the pathological focus at the root apex.
- Radicular cyst in the apical part of the root.
- Severe tooth destruction by caries, which makes prosthetics or restoration using a core insert impossible.
- Longitudinal root fracture.
- Retention or dystopia of an element of the dental system.
- Supernumerary teeth.
- Odontogenic inflammatory process in adjacent structures (trigeminal neuritis, osteomyelitis, sinusitis).
Each patient knows what the reason for removal is in his particular case, but does not always understand how this affects the rate of tissue healing. Let's explain this with a few examples.
In an acute purulent-inflammatory process, there is already a focus of infection in the tissues surrounding the surgical wound. In addition, the tissues are inflamed even before surgery. A similar situation is observed with odontogenic osteomyelitis, inflamed radicular cyst, and odontogenic sinusitis. Obviously, the presence of an infectious-inflammatory process does not contribute to healing after surgery.
We suggest you read How to fix a gummy smile
The gums will take longer to heal after tooth extraction due to infection. The risk of infectious complications increases significantly, as does the risk of bleeding from a postoperative wound. A course of antibiotics is prescribed not so much to prevent infection, but to suppress the pathogenic microflora initially present in the wound.
We see a different situation when removing impacted or dystopic teeth. Retention is incomplete teething, in which the crown does not rise above the gum at all, or only a small part of it rises. Dystopia is abnormal tooth growth, for example, at an abnormal angle, in the direction of an adjacent element, outside the alveolar arch. Such problems are most typical for wisdom teeth.
Impacted and dystopic teeth can generally be absolutely healthy. There are no carious cavities in them, there is no infection in the surrounding tissues. Initially, the situation is more favorable, because pathogenic microflora can penetrate into the wound only from the oral cavity. This can be counteracted by following your dentist's recommendations.
Despite the ambiguity of the situation, the gums heal faster after wisdom tooth removal. The risk of undesirable consequences is lower than after extraction of elements affected by infection. The above is also true for supernumerary teeth. They are always deleted; there are no exceptions to this rule.
Where do scars come from?
Heart scars form where muscle fibers have ruptured or large numbers of cells have died. The body compensates for the damage as quickly as possible - the protein fibrin is produced, which fills the damaged area. What causes lead to heart injuries:
- Thrombosis and vascular embolism. About 45% of the population over 40 years of age already have pathological changes in the blood vessels of the heart. Even the initial stage of atherosclerosis, combined with increased blood clotting, can cause thrombosis, in which a clot of coagulated blood seals the vessel bed. Some cells that do not receive the necessary oxygen and nutrients die, and local tissue necrosis occurs. Such damage poses a threat to the body, so healing occurs very quickly and with fibrotic changes in the tissue. The extent of damage to the contractility of the organ depends on the area of scar growth. An ECG helps diagnose early irregularities in heart rhythm, in particular arrhythmia. For a more detailed study of the coronary vessels, in addition to the ECG, Doppler ultrasound is prescribed. Doppler sonography shows not only the condition of the coronary vessels, but also stenosis of the aorta or inferior vena cava.
- Myocarditis. This is a group of diseases in which inflammation of the myocardial muscle tissue occurs due to infection, allergy, or other reason. Myocarditis often provokes dilatation, in which the volume of the heart chambers increases, but the thickness of the lower or lateral wall remains the same. As a result of dilatation, the heart quickly wears out and receives microtrauma in the area of the wall aneurysm. Tears and focal necrosis of the wall are replaced by fibrous fibers. The results of an ECG can reveal disturbances in the rhythm or strength of heart contractions.
- Ischemia. This is a disease in which the coronary vessels cannot meet the heart's need for oxygen, resulting in chronic oxygen deprivation. Ischemic disease often occurs with damage to the ventricles, with atrophic changes in the posterior or lower wall of the heart, and with myocardial fibrosis (especially in the area of the coronary artery). A natural consequence of ischemic disease is a heart attack. An ECG during ischemia often reveals pathological changes in the walls of the left ventricle; for a more detailed picture, ultrasound dopplerography is used.
- Heart attack. According to cardiologists, this reason is the most popular and most often provokes cardiosclerosis. A heart attack is not always accompanied by a typical clinical picture; in some people it is asymptomatic, and only an ECG can show what happened. Fibrosis in the myocardium, ventricular walls, or interventricular septum increases the risk of recurrent infarction by 45%.
A separate item can be highlighted myocardial dystrophy, that is, a condition in which the muscles of the myocardium and pericardium have atrophic changes; they are thinner and weaker than they should be according to the anatomical norm. Leads to myocardial dystrophy:
- amitaminosis;
- lack of potassium, calcium or magnesium;
- obesity;
- excessive physical activity, irrational sports;
- diseases of the endocrine system, as well as kidneys and liver.
Patients who have at least one blood relative affected by diseases of the cardiovascular system must undergo an ECG and examination by a cardiologist once a year. An ECG can prevent dangerous fibrosis of the left ventricle, protect against heart attack and premature death.
Advice! The cardiologist should be informed about existing endocrine diseases and family history. This information is important for proper prevention or treatment.
How to remove a scar?
The symptoms of heart scars directly depend on the disease that caused them. Within 5-10 years, fibrous replacement can occur without specific symptoms, as long as the heart manages to compensate for the volume of connective tissue and maintain contractility. Then the complaints appear:
- for chest pain;
- for shortness of breath;
- for complete or partial intolerance to physical activity;
- swelling of the face and limbs;
- for rapid fatigue.
The tips of the fingers and toes acquire a characteristic bluish tint, which signals heart failure. Treatment at this stage is aimed at protecting the heart from further damage; surgery or special medications (except cardioprotectors) are not required.
If a heart attack occurs as a result of ischemia or atherosclerosis, extensive fibrosis develops after necrosis, affecting the posterior wall, coronary vessels, often even the aortic valves. In this case, urgent drug treatment is started, which includes:
- beta blockers;
- acetylsalicylic acid;
- diuretics;
- metabolites (ATP and others);
- nitrates.
It is strictly prohibited to select medications on your own after a heart attack; you should contact your cardiologist for detailed prescriptions. Treatment should be continued until the relative normalization of well-being, not forgetting that cardiosclerosis increases the likelihood of a recurrent heart attack by 50-75%.
Fact! The scar after a heart attack continues to increase in area for 2-4 months, all this time it is necessary to maintain dynamic monitoring of the patient. Surgery may be required if the condition suddenly worsens.
Other recommendations from cardiologists regarding the treatment of fibrotic changes:
- do not overload the heart, avoid active sports and physical activity;
- remain calm, avoid emotional stress;
- support the heart muscle with a special diet.
After a heart attack, it is useful to undergo treatment in specialized cardiac centers rather than at home, this helps reduce the damage resulting from impaired blood supply to the heart muscle.
Interesting! If scars on the heart affect more than a quarter of the total volume of the organ, this is an indication for surgery.
Life after heart surgery
How to properly spend the postoperative period, what to be prepared for and what to be wary of.
Heart surgery is a chance for a successful continuation of a normal, full life. The realization of this chance largely depends on a properly conducted postoperative period. It will not be easy for the patient and his family at first, but if everything is done correctly, the result will exceed all expectations. The main principle is not to make sudden movements: all “pre-operative” activity will have to be restored calmly and slowly.
Emotions
Almost everyone experiences mood swings after open heart surgery. Joyful excitement after recovery from anesthesia is often replaced by depressive irritation. Memory weakens, concentration decreases, and absent-mindedness appears. Neither the patient nor his relatives need to worry about this. These symptoms usually go away within a month after surgery.
Home!
Usually you are discharged from the hospital 7-14 days after surgery. The patient must remember that even if everything was successful, it will take him from 2-3 months to a year to fully recover after the operation. You need to start taking care of yourself right outside the hospital. There are many cases where the patient had to be returned by ambulance within 3-6 hours after discharge. If the journey home takes more than an hour, you must stop and get out of the car. Otherwise, serious problems with blood circulation in the vessels are possible.
At home, we must try to build relationships in such a way that the postoperative period is as smooth as possible for both the patient and his family members. Family members should treat the patient with understanding and make efforts for his recovery, but this does not mean that their entire life from this period should be subordinated only to him. Neither the patient himself nor his loved ones need codependency
It is imperative that the patient is constantly monitored by the attending physician after discharge - a family doctor, internist or cardiologist.
What (not) is
Immediately after surgery, your appetite is most likely not very good, and healing physical and mental wounds requires good nutrition. Therefore, it is possible that for 2-4 weeks doctors will not set food restrictions at all. However, within a month, serious dietary restrictions will begin - on fats, cholesterol, sugar, salt, and calories. It is advisable to eat food with a high amount of easily digestible carbohydrates (vegetables, fruits, sprouted grains) and fiber. To combat anemia, you will most likely have to eat foods high in iron: spinach, raisins, apples, moderately lean red meat.
Diet for the rest of your life:
- Lots of vegetables and fruits
- Porridge, possibly with bran, or muesli and cereal for breakfast
- Sea fish as a main dish at least 2 times a week
- Fermented yogurt or juice instead of ice cream
- Only dietary dressings, olive oil and mayonnaise for salads
- Herbal and vegetable spices instead of salt
- Reduce weight to normal, but not quickly. 1-2 kilograms lost per month is ideal
- Move!
- Check your sugar and cholesterol regularly
- Smile at life!
Postoperative sutures
There will definitely be discomfort at the incision site after the operation and will only go away with time. When the stitches are overgrown, pain-relieving ointments and moisturizing lotions can be used to relieve discomfort. It is best if the patient consults his surgeon before using any ointments. If you are concerned about the cosmetic consequences of the operation, then it is advisable to see a plastic surgeon immediately after removing the stitches.
If the postoperative sutures heal normally, 2 weeks after the operation you can take a shower (not a bath, especially not a jacuzzi!). But at the same time: no expensive shampoos and contrasting changes in water temperature. Wash with plain soap and get wet (do not wipe, but blot with a clean towel). It is best for the first “water procedures” after the operation to be accompanied by someone close to you: you never know what can happen….
You should call your surgeon immediately if you experience the following symptoms:
Source: ru.likar.info
Surgical care for scars
In extremely severe cases, an operation is used in which a pacemaker or a cardioverter-defibrillator is installed to maintain the normal rhythm and conduction of the heart. Several more types of surgical intervention that are used for cardiosclerosis:
- Living heart transplantation from a donor. The operation is performed on people under 65 years of age without a history of serious diseases of the internal organs (which is rare, given coronary artery disease or atherosclerosis).
- Bypass surgery is an expansion of the lumen of narrowed coronary vessels. The operation is performed for severe atherosclerosis.
- Removal of the aneurysm. The bulge most often forms in the posterior wall or in the area of the left ventricle. The operation takes place under general anesthesia and consists of truncation of the protruding area.
Surgery is used as both conventional and palliative treatment. The scar after the intervention usually does not pose a threat compared to existing fibrosis.
We will be very grateful if you rate it and share it on social networks