Lichen planus is a chronic and systemic disease. The disease affects the skin and mucous membranes, as well as nail components. It is characterized by immune dependence and is characterized by an inflammatory-dystrophic course. Manifestations of the disease are very diverse.
Among skin diseases, lichen ruber occurs in 0.78-2.5% of cases, the percentage of localization in the oral mucosa is up to 40%.
Varieties and atypical forms
Within the standard classification, there are six types of disease:
- Classic adult - the most widespread (more than half of all cases). It is characterized by rapid development: in a matter of weeks, the rashes become numerous. Sometimes erythroderma may develop. Although the disease is severe, due to which patients sometimes even find themselves temporarily unable to work, it passes faster than the chronic form - in the vast majority of cases, remission occurs in no more than three years.
- Atypical adult - characteristic of approximately 5% of patients with this disease. Its manifestations are similar to vulgar ichthyosis, and proceeds slowly. Treatment is complex and, without treatment, does not go away for decades.
- Classic juvenile - unlike type I, the disease begins in children. It is easier to tolerate than type I (although there are severe cases), and remission most often occurs within a year.
- Limited juvenile - develops in children starting from three years of age. It is distinguished by a clear localization of the affected areas and does not transform into the classical type. The disease can progress in different ways: in about a third of cases it goes away three years after the onset, in the rest it becomes protracted; It may not manifest itself at all or have pronounced periods.
- Atypical juvenile - observed in newborns, is hereditary. The course of the disease is chronic.
- HIV-associated - can occur at any age, is similar in symptoms and course to type I, but has a poor prognosis. May be the first sign indicating HIV infection. Sometimes HIV-associated follicular syndrome occurs.
This is the classification adopted by the Russian Society of Dermatovenerologists and Cosmetologists, but there are others.
According to the classification accepted in Europe, only three forms are distinguished:
- Classical - it combines types I and III from the previous classification.
- Limited juvenile - combines types II and V.
- HIV-associated.
In addition, the existence of intermediate variants cannot be ruled out, due to which the exact type of disease cannot be determined.
Types of pityriasis pilaris
In addition to the main type, there are other lichens that can affect areas of the skin with hair, these include - red lichen, pink lichen (Zhibera), ringworm.
- Ringworm is often an autoimmune reaction of the body, due to the use of medications, or due to the presence of diseases such as hepatitis C.
- Pityriasis rosea is one of the manifestations of an allergic reaction of the body; this type is not contagious, but cases of zoster affecting the whole family have been recorded.
- Ringworm is an infectious disease caused by fungi. The disease is contagious.
Prevention of pilaris
All diseases are easier to prevent, but following simple rules of prevention can contribute to a speedy recovery:
- Do not neglect the rules of personal hygiene, take a shower in a timely manner, do not use other people’s personal hygiene products such as a comb, towel, slippers;
- Do not use detergents with aggressive components that can disrupt the body's barrier functions;
- Avoid frequent injuries, and if there are wounds, treat them with antiseptic drugs;
- Use clothes made from natural fabrics;
- If you have an allergy, try to remove or replace the provoking factor;
- Increase immunity and maintain its functions;
- If there are acute or chronic diseases, treat them completely;
- Do not abuse the solarium;
The duration of the disease varies from two months to a year; timely treatment and strict adherence to the doctor’s instructions will speed up recovery. To prevent a relapse, it is advisable to retake tests a couple of months after recovery and repeat the course of vitamin therapy.
Treatment with folk remedies
The effectiveness of traditional treatment for Devergie's disease remains a big question, but some approaches can complement the main treatment well. In particular, drinking carrots or carrot juice, lotions with carrot or beet juice.
It is recommended to use rosehip oil (containing a large amount of vitamin C can have a positive effect on the course of the disease), chamomile and oak bark are used to prepare infusions, they are used in the form of baths, which helps reduce the severity of the inflammatory process in the dermis.
There is evidence that tar or ground sorrel (when used externally) has a positive effect, however, the use of any folk method should only be an addition to the main therapy.
Ringworm Devergie treatment
At the moment, there are no regulations for the treatment of pityriasis versicolor pilaris, so a combination of medications and physiotherapy is used as a basis.
Ketoconazole cream for lichen
The main part of the therapy consists of administering to the patient the maximum permissible doses of vitamins, especially A and E. The skin surface is treated with medical exfoliating pastes, salicylic acid or birch tar, which help to quickly clear it of scales and nodules.
If fungi of other groups have been identified, treatment is supplemented with daily treatment with broad-spectrum creams: Ketoconazole, Clotrimazole, Terbifin or Lamisil. Nails can also be treated with medicinal varnishes or ointments such as Mikoderil or Loceril.
Devergie's lichen can be easily cured with the help of simple physiotherapy procedures available in clinics:
- phototherapy;
- UV irradiation;
- heliotherapy.
At home, you can supplement the treatment with baths with sea salt, decoctions of chamomile, string or calendula.
In the warm season, patients are recommended to spend more time in the open sun and visit seaside sanatorium resorts. Tatyana Aleksandrovna Pukhova
Dermatologist , 14 years of experience.
Generalist specialist. Engaged in the diagnosis and treatment of diseases of the skin, nails, scalp, as well as sexually transmitted diseases.
Education: 2006 Diploma in General Medicine, Perm State Medical University
Advanced training courses: 2011 “Pillings of superficial-medium impact” 2013 “Plasmolifting in cosmetology and trichology” 2014 “Dermatovenereology”, South Ural State Medical University
Diagnosis of mycosis
Physiotherapy for Devergie's lichen
Devergie's lichen is often “masked” as eczema, psoriasis or ichthyosis. Given the rarity of the disease, some dermatologists and mycologists cannot draw conclusions without extensive histological examination. To do this, a section of skin with a changed surface is taken, which shows damage to the follicles, fatty mouths and hair roots.
In addition, the patient must undergo the following procedures:
- taking a scraping, which helps to identify hidden bacterial infections in the cells of the epidermis;
- examination under a special Wood's lamp;
- Ultrasound of subcutaneous tissue;
- examination of scrapings from the nail plates;
- detailed blood test for the content of certain vitamins and hormones.
Additionally, samples are taken for allergic markers. Additionally, work can be done with a geneticist who determines the presence of a defective gene.
Etiology and pathogenesis
The causes of lichen pilaris are still unknown. Scientists disagree on the etiology of the pathological process. The dominant theory for the cause of Devergie's disease is a hereditary predisposition that is transmitted in an autosomal dominant manner.
In addition to this theory, as a result of studying the infiltration of papules using the immunoblogging method, it was found that there are changes in keratin that are characteristic of other dermatoses - a dysfunction of keratinization, which is observed in ichthyosis, and an enhanced process of proliferation of keratinocytes, as in psoriasis. Many patients suffering from Devergie's disease (lichen pilaris) also have disturbances in the activity of immune system cells - a decrease in the level of T-helper cells and an increase in the number of T-suppressor cells.
According to statistics, the incidence of lichen pilaris is not gender dependent, that is, the disease affects both men and women. There are also no age limits - the incidence range is from 5 to 75 years. Lichen pilaris is characterized by a long-term, often up to ten years, chronic course.
Causes
The exact reasons for its origin are unknown. The main theory is hereditary predisposition. One of the probable factors is a violation of vitamin A metabolism. Presumably, there is a connection with autoimmune diseases (impaired functioning of the immune system).
The development of the disease in some cases is associated with infectious pathologies and malignant tumors.
Ringworm Devergie symptoms
Pityriasis versicolor pilaris
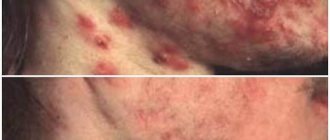
The main symptom of Devergie's lichen is a special lesion in which the follicular form of keratosis appears. It is characterized by inflammation of microscopic openings in the epidermis, which normally secrete sebum or contain the roots of vellus hair. They turn into dense red nodules, resembling “goose bumps” in appearance. If you run your hand over such an area, you can feel the “grater” effect.
The entire affected area by this form of mycosis is covered with whitish peeling, on the surface of which weakened twisted hairs are visible.
Favorite places for this type of red lichen are:
- hair on the head;
- nails and phalanges of fingers;
- forehead and cheeks;
- neck area;
- upper back and chest;
- elbows or knees.
The smallest nodules can merge into large red spots covered with hard, large, flaky scales. The latter strongly resemble bran, with which the official medical name for mycosis is associated.
At an advanced stage, the skin becomes dry and covered with cracks, causing pain when moving or touching.
Devergie's pilaris on the arm
If the disease affects the toenails or fingernails, they become thickened and covered with deep grooves. With the slightest pressure, the patient experiences pain and discomfort. The stratum corneum resembles small spines or cones that form on the entire surface of the plate.
When lichen is localized in the hair growth area on the head, the skin becomes covered with a large number of scales, dense to the touch, which merge into crusts. Visually, they resemble manifestations of seborrhea or psoriasis, so many parents mistakenly ignore the seriousness of the disease and self-medicate.
Pityriasis versicolor pilaris Devergie is almost impossible to identify by external signs even for an experienced specialist. It can be mistaken for ordinary microsporia or trichophytosis on the head.
There are frequent cases of self-healing and complete disappearance of the disease for several months or years, which is especially typical for the congenital form. Relapse occurs under the influence of several factors and always requires careful study for a correct diagnosis.
Acquired Devergie disease
In adults, the disease most often appears in old age, in which case it is considered to be acquired. The acute course is characterized by the appearance of rashes, increased body temperature, and general weakness, but the phenomena regress as quickly as they appear.
The chronic course of dermatosis is observed much more often; changes almost always develop slowly, gradually progress, but are very difficult to treat. Periods of remission and exacerbations follow each other, in some cases remission or complete recovery occurs suddenly even without treatment.
Where are changes defined?
With Devergie's disease, there is no specific localization of the pathological process on the skin. Most often, changes are found in the area of the elbows and knee joints (usually on the outer surface). Although rashes can also be found on the scalp (hairy part), on the face, back, stomach or any other parts of the body. But even in the most severe cases, unaffected areas of the skin remain.
Quite often, changes are observed on the skin of the palms and soles (unlike Kirle’s disease - keratosis, in which there are always no changes with such localization). In this regard, Devergie's disease is similar in its manifestations to Reiter's syndrome , in which palmar hyperkeratosis can also be observed.
Nails are often affected, there is thickening of the nail plates, the appearance of longitudinal and transverse grooves, this disease is similar to nail psoriasis, in which onychodystrophy is also observed, but the nails are pinpoint affected, and therefore look like a thimble.
The mucous membranes of pityriasis versicolor pilaris are not affected in most patients, but in rare cases, cone-shaped thickenings on the mucous membrane of the palate or areas of hyperkeratosis on the mucous membrane of the cheeks may be observed, which can easily be confused with leukoplakia .
How is Devergie's disease treated?
Therapy is based on the use of large doses of vitamin A, 100-200 thousand units per day are prescribed, the minimum course is two months, after which it is recommended to take the same break, then repeat the course if necessary.
Multivitamin complexes or individual B vitamins and vitamin E are prescribed in addition; their use, as a rule, gives good results.
Retinoids (Roaccount) have also proven themselves to be effective in the fight against this pathology, but the decision to use them is made by the doctor after making an accurate diagnosis.
Drug therapy is recommended to be supplemented with PUVA sessions (usually the course consists of 10 sessions), such treatment is carried out in severe cases of pathology and in the absence of contraindications, and physiotherapeutic methods of treatment such as phonophoresis with glucocorticosteroids are also used.
For local treatment, preference is given to ointments with vitamin A; ointments based on acetylsalicylic acid are widely used to eliminate inflammatory phenomena in the skin. In cases of severe inflammation, ointments with glucocorticosteroids are used; in extreme cases, systemic glucocorticoids are prescribed.