Why don't systemic antibiotics cure acne?
1. Hyperproduction of sebum.
The increase in the level of sex hormones, which is usually observed during rapid puberty, increases the secretion of sebum. 2. Pore blockage. Skin pores become filled with oil, bacteria, and dead skin cells. This can be seen in the form of unsightly white and black dots on the skin. 3. Growth of bacteria. Hundreds of species of bacteria live on our skin and interact with it all the time, starting from birth. Overproduction of sebum and other factors spur their growth. 4. Inflammation. Excessive growth of bacteria initiates an inflammatory process in the skin, which results in those terrible pimples that bring a teenager to the doctor's office.
“Systemic antibacterial drugs help us control the growth of bacteria, but we do not influence other factors, so acne cannot be cured with antibiotics alone. But we have a lot of potentially serious side effects associated with long-term antibiotic therapy,” explains Dr. Tamburro.
Antibiotics for back acne
Most often, a rash on the back is formed due to hormonal imbalances, gastrointestinal problems, weakened immunity, lack of vitamins in the body and stressful situations.
If, with a mild degree of back damage, you can use traditional medicine and prepare herbal decoctions, then with moderate and severe forms, stronger drugs should be used.
If acne affects small areas of the skin, the patient is prescribed antibiotics in Unidox
, and for external use -
Zinerit
.
For confluent formations and a large area of rashes, Roaccutane
, which has an anti-inflammatory and healing effect on the skin.
For external use, use Airol
, which is available in the form of gel, cream and lotion.
Solcoseryl is used to treat acne wounds.
or
Argosulfan
.
Before using these medications, you should treat the skin with Chlorhexidine
or
Furacillin
.
Acne - causes and mechanism of development
Under the surface of the skin there are many hair follicles, from which hair grows and penetrates the surface of the skin through its pores (Fig. 7a). At the base of each hair follicle there are many small sebaceous glands that produce sebum. This fat comes from the sebaceous glands through narrow channels, first into the lumen of the hair follicle, and then (along the hair shaft) it rushes out to the surface of the skin.
The development of acne is associated with two points:
- Strengthening the function of the sebaceous glands at the base of the hair follicles - increased sebum production is directly related to the increased production of androgens (male sex hormones) by the adrenal glands. These hormones are produced in both sexes, but to a lesser extent in women. This is why acne develops during puberty in teenagers.
- Epithelial keratosis within the follicle - the surface of each hair follicle is covered from the inside with layers of epithelial cells. An increase in the rate of exfoliation of epithelial cells from the inner surface of the follicle leads to an increase in the number of exfoliated dead cells in its lumen.
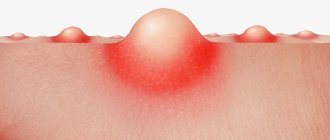
Increased sebum production and an increase in the number of desquamated cells lead to the formation of plugs that clog skin pores (Fig. 7b). It is these plugs that are called acne vulgaris. Blackheads may look: → in the form of white bumps, if the plug forms deep in the pore (Fig. 9), → in the form of black dots inside the pores, if the plug forms at the surface of the skin (Fig. 10).
The formation of plugs leads to the fact that the sebum constantly produced by the sebaceous glands cannot come out and accumulates in the lumen of the hair follicle (Fig. 7b). A closed space with a nutrient medium inside is an ideal place for the development of infection, and therefore bacteria that have entered the hair follicle from the surface of the skin begin to multiply intensively there.
This leads to the development of inflammation in and around the follicle. Inflammation can occur for a long time without the formation of pus; in this case, such a formation is called a papule (Fig. 10). A papule looks like a red, inflamed bump on the surface of the skin. Papules can disappear without a trace over time, but usually they transform into pustules. The pustule is already a classic pimple with pus inside (Fig. 11).
In addition, with more severe forms of acne, large inflammatory formations - nodules and cysts - can form. The nodules are large, dense, painful papules, which also have no pus inside (Fig. 12). Cysts, as a rule, arise when an attempt is made to squeeze out pimples located deep in the skin, as a result of which pus penetrates deeper into the tissue (Fig. 13).
List of popular medications
Antibiotics for acne are prescribed by a dermatologist. The doctor diagnoses the patient’s health status and prescribes a set of tests (blood and urine tests, bacterial culture of inflammation contents). Preparations are divided into internal and external use, bactericidal (complete destruction of bacteria) and bacteriostatic (stopping the proliferation of bacteria) action. Depending on the state of health, the doctor prescribes ointments and tablets for local or general acne.
Effective treatment of acne occurs through the use of antibiotics of three groups:
- The tetracycline group is designed for use in low doses, which avoids adverse reactions. A special feature of the drugs is that they increase the body’s susceptibility to the influence of ultraviolet radiation. Therefore, during the treatment process, visiting a solarium, staying in the sun for a long time, or undergoing physiotherapeutic treatment is unacceptable;
- The macrolide group of drugs is used in combination with zinc ointment. During treatment with macrolide medications, the consumption of dairy products is prohibited. It is also important to adhere to the diet established by a dermatologist on an individual basis;
- Linkosamine group. Taking medications requires strict medical supervision. The course of treatment is about ten days. Medicines should not be combined with other medications.
When taking antibiotics, it is necessary to take drugs that normalize the intestinal microflora (Linex, Hilak Forte, Normolax, Lactusan, activated carbon), or fermented dairy products: kefir, yogurts, etc.
The list of drugs for external use includes the following medications:
- Gels “Klindovit”, “Klitndadop”, “Dalacin” are based on antibiotics of the lincosamide group. The drugs help destroy bacteria from the inside. The gel should be applied to the affected areas 2 – 3 times a day. The course of treatment ranges from 4 weeks to 6 months.
- Anti-acne ointment “Deriva-S”, “Klenzit-S” . Its base is adapelene. The substance is characterized by anti-inflammatory and sebostatic effects. Ointments have an effect on hyperkeratosis and have a gentle but effective effect on comedones. The course of treatment is about a month.
- Duak-gel gel is developed on the basis of the antibiotic clindamycin, which destroys the early stages of protein synthesis, benzoyl peroxide, which controls the production of sebum.
- Anti-acne cream “Zinerit” has a bacteriostatic effect, reduces the production of sebaceous gland secretions. Apply twice daily. The course of treatment is at least 1 month.
- “Isotrexingel” inhibits the activity of the sebaceous glands, reduces sebum production, and reduces the inflammatory process. The course of treatment is about two months.
In addition, the following ointments can be used.
The fight against acne will give results after a comprehensive effect on inflammation of the skin. This includes regular cleansing of the epidermis and a properly selected course of antibiotics.
The list of drugs for internal use includes the following medications:
- "Erythromycin" destroys bacteria and microbes, blocks the production of protein in bacteria. The drug soothes inflammation and helps cleanse the skin. Eliminates scars and dark spots after acne localization. Recommended for use in purulent inflammatory processes. The tablets are coated, which dissolves in the intestines. Take several times a day with an interval of 4 - 6 hours (the dosage and time of administration are determined by the doctor).
- "Levomycetin" helps inhibit the growth of microbes at the cellular level. The active substance destroys protein synthesis and reduces the production of sebaceous glands. The drug is effective in the treatment of staphylococci, enterococci, pneumococci. The course of treatment lasts on average 10 days. The frequency of administration is 4 times.
- Metronidazole is an antimicrobial and antiprotozoal medicine. The active substance penetrates the cells, disrupts the respiratory chain of protozoa, which contributes to the death of pathogenic formations.
- "Tetracycline" is a broad-spectrum antibacterial drug. It is characterized by effective fat solubility, therefore it quickly copes with excessive secretion of the sebaceous glands. The course of treatment is several months. Take 4 times a day 30 minutes before meals. The minimum daily dose is 1 g per day.
- Doxycycline capsules are active against aerobic cocci, spore-forming and non-spore-forming cocci. Penetrating into the body, the drug affects pathogens inside cells. The course of treatment is 2 – 3 weeks. The minimum dose of the drug per day is 1 g.
- Minocycline prevents the spread of bacteria and interferes with the synthesis of bacterial proteins. The course of treatment is 15 days.
- "Ciprofloxacin" destroys protein synthesis in cells; the active substance effectively affects reproducing microorganisms, as well as bacteria that are at rest. It is recommended to take 250 mg twice a day. The course of treatment is from 7 to 10 days.
- "Lincomycin" has a bactericidal effect: it reduces inflammatory processes of various types, helps destroy bacteria that provoke the spread of infection, and corrects the production of sebaceous secretions. The dosage and duration of treatment is determined by the attending physician.
Taking medications begins with a high dose, gradually moving to low maintenance doses.
The video shows additional means of combating skin inflammation:
Antibiotics for acne –
It is known that doctors’ commitment to prescribing a particular antibiotic depends on geographical, historical conditions, and information and educational programs. Thus, the choice of antibiotic and the principles of its prescription differ in the USA, Great Britain and continental European countries. Among systemic antibiotics for the treatment of acne, the group of tetracyclines (tetracycline, doxycycline and minocycline) and the group of macrolides (erythromycin) have the most evidence regarding clinical and microbiological effectiveness.
Tetracycline group drugs remain the priority among systemic antibiotics for the treatment of acne. Doxycycline is characterized by higher microbiological and clinical efficacy compared to tetracycline.
Currently, it is used less and less due to the increasing resistance of microflora and the high frequency of unwanted drug interactions.
The duration of systemic antibiotic therapy can reach 24 weeks or more with mandatory monitoring of results every 4 weeks. In clinical practice, it is advisable to combine oral antibiotics with external agents containing retinoids or benzoyl peroxide. If there is no dynamics of the process, alternative therapy with systemic retinoids (isotretinoin, Aknetin) should be prescribed.
SIDE EFFECTS - with antibiotic therapy with tetracyclines or macrolides, side effects from the gastrointestinal tract (colitis and diarrhea) occur in 5% of patients, candidiasis (vaginal) - in 6% of women. Other complications include onycholysis (doxycycline), ulcerative esophagitis (doxycycline), persistent exanthema (tetracycline and erythromycin), photosensitivity including porphyrin-like changes in the skin (long-term tetracycline therapy), phototoxic rash (doxycycline), liver dysfunction and changes in clinical analysis blood (tetracyclines and erythromycin).
Choosing the optimal effective antibacterial drug for the treatment of acne is a very difficult task. Often the choice is based on the personal preferences of the clinician, taking into account the brand name, the medicinal base of the drug, its form (solution, gel, cream, ointment), cost and effectiveness of treatment.
It should be remembered that the main problem of long-term use of antibiotics is the development of persistent microbial resistance, so the persistent prescription of more and more new antibiotics to patients with acne who do not show clinical improvement after antibiotic therapy is unjustified. To improve the effectiveness of acne therapy, information regarding the global/regional status of microbial resistance to that drug should, if possible, be used before prescribing a specific systemic antibacterial agent.
Currently, we know much more about acne than we did 5-10 years ago. Specialists have a number of effective medications from different groups in their arsenal, but, unfortunately, none of the modern treatment methods can guarantee the absence of relapses of the disease in the future. It is important to regularly adjust the prescribed treatment and dynamic follow-up monitoring of the patient even after achieving clinical remission.
A delicate issue for the fair half of humanity is the removal of facial hair, in particular in the area: neck, upper lip, as well as temples, eyebrows, forehead line, chin, cheeks - laser hair removal solves this problem once and for all.
Antibiotic anti-acne medications successfully cope with skin inflammation of any complexity. On the other hand, along with the pathogenic microflora, the beneficial microflora is destroyed, so immunity is reduced. For this reason, it is not recommended to self-medicate. Below are some reasons against using antibiotics:
- Most drugs negatively affect the functioning of the liver, as a result, a large amount of toxic substances accumulate in the body;
- Antibiotics can cause allergic manifestations (dysbacteriosis, candidiasis), the use of drugs is individual. The cause of allergies is the aggressive effect of antibiotics on pathogenic and beneficial microflora. In this regard, it is recommended to take antibiotics together with antifungal and prebiotic drugs;
- The drugs often cause dizziness, loss of balance while walking, discoloration of teeth, and sensitivity to ultraviolet radiation.
- It is important to choose the right dosage and duration of medication.
Drugs of this pharmacological group have the following effects on skin with inflamed acne:
- Bacteriostatic effect. This means stopping the further growth of pathogenic bacteria.
- Bactericidal effect. Medicines completely destroy bacteria.
- Reduces fatty acid levels. Their content is reduced by 2 times.
- Suppress the mobility of neutrophils during the inflammatory process.
There are 2 groups of antibiotics:
- External. They are applied either to the entire acne-affected skin, or locally to each pimple, depending on the preparation.
- System. They are taken orally, and the medicine acts entirely on the entire body. The tablets have an effect on the stomach, and when administered subcutaneously, intramuscularly or intravenously, the medicine bypasses the gastrointestinal tract.
Firstly, a course of treatment is prescribed only after a diagnosis is made. Secondly, many factors must be taken into account (the cause of the disease, the severity of the disease, etc.).
Despite the fact that ointments, creams and gels for acne are sold freely in pharmacies, they should also be prescribed by a doctor. The fact is that each of these drugs is aimed at combating a specific type of acne. Only a doctor can determine which type of bacteria has affected the patient’s skin and which bacteria is the causative agent of the disease. The most effective means are:
- Gel "Baziron". Aimed at treating acne caused by the bacteria Propionibakterium acnes or Staphylococcus epidermidis. The gel is applied exclusively to the pimple, as it can cause burns to healthy skin.
- Ointment "Zinerit". Contains erythromycin, which is considered the most effective component in the fight against acne. Girls love this ointment very much, because you can apply makeup on it.
- Cream "Differin". It contains a retinoid, which is also effective against acne. This remedy is especially indicated for those who are predisposed to post-acne, that is, spots after acne. In addition, the cream also lightens existing marks. You only need to apply the cream at night.
- Gel or cream "Skinoren". Contains azelaic acid. A very effective remedy.
- Gel "Curiosin". Contains hyaluronic acid and zinc. The gel effectively fights acne, but does not dry out the skin and promotes its nutrition and regeneration.
Antibiotics for acne are most often used externally (as part of creams and gels), less often - in the form of tablets. Gels with antibiotics are prescribed for all forms of acne, except for the form when there is only acne without inflammation. And under no circumstances should you use ointment forms of antibiotics!
- Antibacterial creams and gels - usually contain antibiotics such as erythromycin and clindamycin. Usually prescribed for acne, mixed acne (acne with pimples). Examples of gels with clindamycin: “Clindovit”, “Dalacin”, “Clindatop”.
There are combination drugs where the antibiotic is combined with drugs from other groups. Such drugs are preferable and stronger, but before using them, you need to consult a dermatologist:→ “Duak-gel” – contains clindamycin and benzoyl peroxide, → “Deriva-S”, “Klenzit-S” – clindamycin and adapalene (retinoid), → “Isotrexin gel” – erythromycin and isotretinoin (retinoid). → the drug Zinerit is an effective combination drug based on erythromycin and zinc.
- Oral antibiotics – tableted antibacterial drugs should only be prescribed by a doctor. They are usually prescribed only for cystic acne. However, oral antibiotics may be prescribed for both acne and acne if standard topical therapy for the latter has not been successful.
Mechanism of action of antibiotics
Antibiotics against acne on the face are bactericidal and bacteriostatic. In the first case, bacteria die, and in the second, the growth of excess microbes stops. If acne appears only on the face, then treatment is carried out with bacteriostatic agents.
They affect microorganisms, causing their death. Some antibiotics act on pathogens by blocking protein synthesis. Subsequent growth of amino acid chains is prevented. To determine which drug is suitable for the patient, resistance is identified.
For treatment to be effective, it is recommended to use the medicine for a certain number of days according to the regimen. If you deviate from the schedule, the resistance of the pathogen to the drug and the effect of treatment are lost. Bacteria form protective mechanisms during the period of absence of the active component of the drug in the body. New compounds are formed that do not react with the prescribed antibiotic. In this case, a new remedy is prescribed.
How to treat acne correctly -
If you are unable to maintain your facial skin in good condition on your own, be sure to consult a dermatologist. Treatment of acne in adults and adolescents is the same, with the exception of women in whom hormonal contraceptives can be used as additional therapy.
How to treat acne will depend primarily on what kind of inflammatory elements are on the skin of the face. Treatment will be different in situations where there is –
- when there are only acne,
- only pimples (papules and/or pustules),
- for mixed forms of acne (acne pimples),
- in the presence of nodules and cysts.
Below you can see a list and description of medications, as well as a diagram (Fig. 14), which shows what needs to be used for each form of acne.
Duration of treatment – in order to achieve any noticeable improvement in the condition of the facial skin, up to 4 weeks of treatment are necessary. The standard course of treatment is about 6 weeks. However, with persistent acne, treatment can take up to four months (and sometimes longer) to get good results and get rid of not only acne, but also post-inflammatory skin pigmentation.
Patient reviews
During adolescence, my daughter developed acne on her face. Since she began to squeeze them out, an inflammatory process began on the skin. We consulted a gynecologist and a dermatologist and prescribed tetracycline antibiotics. The pills were taken according to the schedule. There were no side effects. The acne disappeared in 2 weeks.
Alena, 39 years old
Using antibiotic ointment for acne on my face, I quickly got rid of the inflammation. The treatment lasted 7 days. The skin condition improved, there were no side effects. After therapy, I followed all the doctor’s instructions, so a relapse was ruled out.
Andrey, 25 years old
When acne appeared on my face, I decided to make a mask with tetracycline.
After just 5 days, the mild inflammation disappeared and the acne disappeared. To prevent a relapse, I used special moisturizers for another 3 days. Irina, 32 years old
Treatment of acne in women -
Oral contraceptives may be used as an adjunct to primary treatment in adolescent girls and women. First of all, this treatment method is recommended for healthy women who also need contraception. Hormonal contraceptives are also prescribed to those women for whom traditional acne treatment methods (described above) do not give good results.
In addition to oral contraceptives, women can also use androgen blocking drugs, for example, Spironolactone. Read more about these treatment methods here.
Mechanism of formation of rashes
Acne develops as a result of infections, disorders at the genetic level, immunosuppression, digestive disorders, neuropsychic stress, and endocrine pathological changes. The disease can occur at any age, in both men and women.
There are 4 factors in the mechanism of development of rashes in the face:
- Increased work of the sebaceous glands. With increased sebum secretion, its bactericidal ability decreases and its concentration changes. Secretory secretions become dense, forming plugs in the ducts, which leads to their blockage.
- Follicular hyperkeratosis, which is based on the disruption of the constant renewal of hair follicles. Together with blockage of the ducts and thickening of the superficial stratum corneum, the secretion of the sebaceous glands increases.
- Reproduction of pathogenic flora. The microbe Propionibacterium acnes can lead to inflammation under certain conditions.
- An inflammatory process in which a response of epithelial tissue occurs.
Classification of acne by human age
Acne can occur at any age, regardless of gender.
Pathology is divided into 2 categories – juvenile acne and age-related acne. Type 1 – acne vulgaris. Occurs in adolescence and young adulthood. Mostly it affects the male part of the population. A distinctive feature is the development of seborrhea against the background of acne.
Classification:
- Papules. Miniature nodules with a red tint. There is no purulent content. This species develops over 12 days, after which it disappears, leaving small traces that discolor and disappear over time.
- Pustules. Dense accumulations, in the center of which there are balls with purulent contents. They form independently or when an infection enters the papules. Over time, they heal, leaving bluish spots.
- Abscess acne. Formed when pustules open. Microscars remain at the site of the outbreak. Most develop in people prone to dermatoses.
- Phlegmonous acne. Flat formations on the surface of the skin with pronounced signs of hyperemia and swelling.