Why are we writing this article
We have been selling lingerie, clothing and medical products for women post-mastectomy for many years. We have a wealth of experience, product training and advice from specialists in this field. During this time, we studied all the details and the level of discomfort that a woman experiences after going through such an experience.
We know for sure that you can regain your previous level of comfort and achieve the desired quality of life. After breast surgery, you can live your normal life and get the same pleasure from it. And we know how to do it.
We want to share our knowledge. And in this article we will tell you what we can offer:
- rehabilitation means with which you can really feel as healthy as possible and look natural and stylish;
- a wide range that we have been honing over the years - we select the most progressive, comfortable and natural products from the world's best manufacturers: exoprosthetics,
- preventative compression sleeves, underwear with pockets, casual clothing, swimsuits;
- Our consultants will teach you how to use and care for these products. And also take care of yourself - they will talk about a gymnastics program to develop your arm and prevent swelling;
- goods of different price categories - for women with different capabilities; a full package of documents and certificates - so that you can receive compensation from the state for the purchase of special goods.
Options: pros and cons
You cannot determine on your own which procedure is one hundred percent right for you. It is necessary to undergo an examination by a doctor, do a series of tests, and make sure about the type of mastectomy (full or partial).
Sometimes, along with the damaged area, correction of the healthy breast is also performed, enlarging the gland or tightening the tissue.
It is important for the surgeon to know about radiation therapy or scars in other areas (abdomen, buttocks, back), and the date of the mastectomy.
How is the procedure done?
Breast reconstruction is usually carried out in two stages and depends on the chosen method.
This is a rather labor-intensive process that requires careful diagnostics and selected materials. The breast is reconstructed using an implant, which is placed under the muscle . Naturally, it is necessary to preserve or restore the breast skin and achieve normal functioning of the muscles (pectoralis and serratus).
Expander
Suitable for both delayed and one-stage breast reconstruction. It is injected into the patient instead of the removed gland, and then gradually (the procedure takes months) saline is injected into it. In this way, it is possible to stretch the skin and fatty tissue, preparing them for the implant. Afterwards, it will be necessary to form the areola and restore the nipple if they could not be preserved after the mastectomy.
Musculocutaneous flap transplantation
If the skin cannot be preserved, a musculocutaneous flap is used for breast reconstruction. Often patients agree to this method in order to minimize complications after surgery and quickly obtain the desired result. In addition, surgeons recommend this method for aesthetic reasons.
To do this, a flap is cut from the patient's back, lower abdomen or buttock. Not only skin, but also fatty and muscle tissue is captured, and then the flap is grafted onto the reconstructed area of the mammary gland. Often the implant is inserted immediately along with the flap so that the breast is formed as aesthetically and naturally as possible. The transplant is best suited for small breast sizes .
- If the flap is taken from the back, complications in motor functions are possible and a noticeable scar will remain.
- The lower abdomen option is often recommended for overweight women; at the same time as breast restoration, it will be possible to get rid of some of the fat deposits and perform plastic surgery on the problem area. However, scars may remain and the blood supply to internal organs and microcirculation may be impaired. The belly button may need to be moved or reconstructed.
- The gluteal flap is the least used flap due to the difficulty of vascular repair. This operation will take a very long time (up to 12 hours, as opposed to 3-5 for the previous ones), but the scar in this area will be less noticeable.
Combined method
If it was possible to preserve the skin and muscles, and the tumor was small, then the missing volume is simply filled with fatty tissue. And the gland itself moves along the chest wall. This method involves reducing breast volume, but you will not have to resort to implants.
A plastic surgeon will be able to correct the shape of both glands (healthy and damaged) so that the breasts look as aesthetically pleasing as possible. Unfortunately, if the damaged area was large, then this method will not work.
Nipple and areola restoration
The nipple and areola are restored during the last stage of breast reconstruction under local anesthesia. The surgeon performs the operation in different ways, the most popular is to take part of the tissue from a healthy nipple. But it is possible to transplant flaps (usually pigmented) from the eyelids and labia.
Recovery may take 3-4 months to achieve symmetry . Areolas are most often painted on fabric using tattooing.
About experiences and complications
The most important thing is behind us - the operation is done. Life saved.
But the feeling of anxiety continues to live. Now for other reasons.
How now, after the operation, will people around you perceive your body? After all, you want to be beautiful and be liked - in the mirror, by the man you love, to be on an equal footing with your friends. I want to live my life as before, and not have anything overshadow the joy of simple things. Just relax and feel as attractive as before. Realize that everything is okay.
And as soon as all these normal desires are formed, embarrassment and confusion immediately appear. Self-confidence as a woman quickly declines. Sadness takes its place.
Yes, there are tasks that can become reality and for which you need to remain fully prepared:
- physical features: lymphedema, uneven suture, partial resection, stiffness, sweating, weight change, spinal problems;
- psychological state: sadness and confusion about what and how to do next.
And here we want to draw attention to the recommendations and products we offer. Because they are designed specifically to restore a woman’s previous comfort and maintain her health.
Relevance of the problem
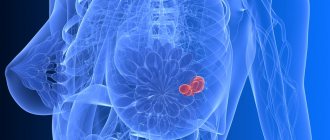
Despite the fact that in recent years oncologists have focused on organ-preserving surgical interventions, the percentage of traumatic operations for breast cancer remains high. Mastectomy (complete removal of the mammary gland) leads not only to physiological changes in a woman’s body, but also to severe psychological problems.
In essence, the patient becomes disabled. She loses her feminine attractiveness and self-confidence. This often leads to significant changes in social and family life. Sometimes neuroses and depression develop against this background. [3], (p. 232 - paragraphs 1 and 2)
The only way out of the situation is plastic surgery to restore the mammary gland. The price for breast reconstruction in private medical institutions, depending on the complexity, is tens and hundreds of thousands of rubles. You can carry out such an intervention free of charge in a specialized surgery department by applying for a quota under compulsory medical insurance.
Postoperative period: what to buy
For the first time after surgery, two products are needed. This is a post-operative prosthesis and bra. In the article we will talk about the best samples - with excellent production quality and high wear resistance.
1. During the postoperative period, doctors advise wearing a primary textile prosthesis. It solves the following problems:
- compensates for volume;
- does not interfere with the healing of sutures;
- protects the skin;
- does not put pressure on the postoperative surface, it can be worn two to three weeks after surgery, until the drainage and bandage are removed;
- The woman individually adjusts the volume of the prosthesis herself.
The prosthesis is suitable for any breast and is adapted for any type of operation:
- radical mastectomy;
- radiation therapy;
- partial resection.
It is used as an overlay for asymmetry and regulates and corrects volume as weight changes.
Perfectly imitates the shape of the breast, due to the compacted molded part of the prosthesis, even if you remove all the filler, the shape of the prosthesis will not change. The product is securely fixed in the bra.
This prosthesis is multifunctional. In the future, it can be used at home - for unloading and replenishing volume. You can sleep, work, and move actively in it. Wearing a primary prosthesis has no contraindications or restrictions. No precautions are required when transporting in travel bags or suitcases. And alternating a silicone prosthesis with a textile prosthesis extends the service life of both products.
2. The second product is a post-operative bra
This product takes into account all the features of the postoperative period. Made from cotton - soft and breathable. And easy to use.
Cups:
- elastic, easily take the shape of both the breast and the postoperative prosthesis;
- The neckline and armhole line are high - the lymph flow is not compressed, postoperative sutures are not visible.
Straps:
- wide, comfortable, softly padded, does not press through the shoulders;
- They do not have length regulators - the strap is elastic and automatically selects the fit on the woman’s back.
Back:
- high, wide, has no fastener;
- allows you to sleep and relax in the bra.
Front clasp:
- comfortable for a woman immediately after surgery - you can put on and take off the bra without assistance;
- With just two buttons and a Velcro fastener, the volume under the bust can be individually adjusted.
In the future, such a bra will be indispensable in the wardrobe for unloading, sleeping and relaxing.
How to apply for a quota
Breast reconstruction under compulsory medical insurance is performed for medical reasons. Therefore, to obtain a quota, you need to consult with your doctor. If the doctor confirms the need for reconstructive treatment for the patient, he fills out a special referral form for hospitalization for the provision of VMP, which is certified by the medical commission.
The following documents are attached to the referral:
- an extract from the medical record in which the doctor describes the indications for reconstructive surgery;
- copies of the patient’s documents (passport, compulsory medical insurance policy, certificate of compulsory pension insurance);
- originals (copies) of all necessary examinations (preoperative tests, statements of treatment, etc.);
- signed consent to the processing of personal information. [2], (paragraphs 13 and 14)
This package of documents is provided to the authorized healthcare organization. A voucher for the provision of VMP is issued for the patient. Next, a special commission decides whether to refer the woman for breast reconstruction or not. If the answer is positive, the patient receives a special notification indicating where and when she can receive the necessary help. [2], (point 18)
Constant wearing: what to buy
There are four types of products that you will need to create daily comfort in your everyday life.
1. Clothes
Blouses, T-shirts, pajamas, shirts, dresses, tops, sports T-shirts - these products are designed to be worn without a bra because they have a built-in - sewn-in bodice with pockets to support and secure the prosthesis.
2. Bras
The underwear is tailored in such a way that, thanks to the high neckline, a complete fit of the prosthesis is ensured, scars and uneven postoperative surfaces are hidden. Cups with pockets are responsible for reliable fixation and correct anatomical placement of the breast and prosthesis in the bra, without direct contact of the prosthesis with the body. Wide, ergonomic straps guarantee the prevention of lymphedema and relieve stress from the neck and shoulders - with a heavy bust. The high armhole hides tissue deficiency in the armpit area and provides wearing comfort. The wide belt under the chest does not put pressure on the diaphragm, ensuring free breathing and eliminating discomfort in the stomach area.
3. Swimwear
Swimsuits are tailored like bras, have a stylish appearance, and can be either separate or one-piece.
4. Dentures for permanent wear for an attractive appearance
Modern prosthetics provide natural sensations and behavior. They are soft to the touch, sway when walking and “fall off” when lying down. Designed with a special thin edge - it provides a delicate fit in the sensitive seam area and a natural transition to the lines of the body.
These products are made taking into account the various features of the female breast: full-bodied and lightweight, triangular and teardrop-shaped. They also minimally touch the body, so they do not overheat it - there is no increased sweating, and a natural microclimate is maintained.
Consultations: ask a question
I invite you to subscribe to our blog on Instagram “MEDICAL REPORTER”>link>
Kremlin. Presentation of the “We Will Live” award in the category “Best Oncologist” to Dr. Skvortsov>link>
You have the opportunity to get a quick answer to your question from Dr. Skvortsov>link>
You have the opportunity to sign up for an online consultation with Dr. Skvortsov>link>
The questions are answered by the winner of the nomination “BEST ONCOLOGIST” Vitaly Aleksandrovich Skvortsov , doctor of the highest category of the State Clinical Clinical Oncology Department, kmn, oncologist surgeon, mammologist, plastic surgeon
I've been wearing an elastic bandage for a month now since my mastectomy.
QUESTION: Good afternoon! After my mastectomy, I’ve been wearing an elastic bandage for a month now; they won’t let me take it off. I have a severe allergy to the bandage, can I replace it with something or not wear it at all? ANSWER: Hello! What are you wearing it for? I don’t see the point of wearing it if it’s to fight lymphorrhea. She will still be there! Discuss this issue with your doctor.
Is the prescribed treatment sufficient for me and can I undergo preventive measures?
QUESTION: Vitaly Alexandrovich, hello! I had a mastectomy of my right breast. IHC: ER, PR =8, Her2neu=3+, Ki67=30%. The oncologist prescribed me to take tamoxifen for 5 years. In the left breast, according to MRI results, there are single foci of adenosis and inflammatory changes in the nipple area. (MS BI-RADS3). Is the prescribed treatment enough for me and can I have a preventive mastectomy of the left breast? Thank you in advance. ANSWER: Hello! There is no point in performing a preventive mastectomy, because it has been proven that the chance of dying from a diseased breast is much higher than suffering from a healthy breast in the future. I don’t agree with the treatment! It really all depends on age. How old are you? What is the pronounced pathology and concomitant diseases? Usually in this case chemotherapy with anthracyclines and taxanes is prescribed, then targeted therapy with trastuzumab and only then tamoxifen! Discuss treatment adjustments with your doctor.
4 months after mastectomy fluid accumulates
QUESTION: My wife had her right breast and lymph nodes removed. I had stage 1 breast cancer; for the past 4 months I have been pumping out liquid with a syringe, now 10 ml. How long does it take to pump out? ANSWER: Hello! Accumulation of lymph in the axillary area is normal and 10 ml is very little, I would not pump it out at all or switch to rare dressings, for example, once a month and then the fluid will stop accumulating. Consult your surgeon, perhaps he will give his recommendations.
After a mastectomy, swelling of the forearm began
QUESTION: Hello, please help! After the mastectomy, swelling of the forearm began. What should I do? It’s the holidays and no one is working. The local surgeon removed the drains and told me to make compresses with vodka. Can I do this? ANSWER: Hello! Compresses are possible, but it’s better to buy a compression sleeve! In general, the forearm cannot swell so sharply, I think that it just seems to you that there is no swelling. The holidays will end and you will contact your surgeon; you definitely need to see yourself; most likely, you have accumulated lymph fluid in the armpit area.
On what day are stitches removed after a mastectomy?
QUESTION: Hello, Vitaly Alexandrovich! On January 20, I had a radical mastectomy. The extract dated January 29 says that the stitches will be removed on the 21st day, on January 30 I went to the surgeon, after dressing, he said that he would remove the stitches on Monday, is this normal? Thank you. ANSWER: This is normal and there is nothing wrong with the fact that the sutures will take longer or be removed earlier; the surgeon visually determines the need to remove the sutures. It is actually better to leave the stitches in longer after a mastectomy.
There is a burning sensation and slight swelling in the suture area
QUESTION: Hello. A month has passed since the mastectomy of the right breast. There is a burning sensation and slight swelling in the suture area. This is fine? ANSWER: Hello! Of course, this is normal in this case. Not enough time has passed that there are no sensations. The mammary gland is a very sensitive organ, although it is not there, but the skin remains in some parts no less sensitive. All pain and other discomfort should go away in 4-6 months.
Preventive mastectomy
QUESTION: Good afternoon! A mutation was discovered in the brca gene, my mother and her two sisters died before the age of 42 from breast cancer. I have fibrocystic mastopathy. I’m 35 years old, have two children, and don’t plan to give birth again. Should I have a prophylactic mastectomy? 80% of getting breast cancer is a big risk. ANSWER: Hello! Prophylactic mastectomy is still illegal in our country; it is performed in two places as part of clinical trials! In fact, prophylactic mastectomy does not solve the problem, since with such mutations cancer can arise in other places! 80 percent is a high figure, very overestimated, in fact, not everything is so bad, I would simply recommend that you be monitored regularly or perform the entire full mutation model and discuss with your surgeon the advisability of a preventive mastectomy!
severe distortion of the spine towards the healthy arm and chest
QUESTION: Hello! It has been 9 years since my breast removal surgery. During this time, the gallbladder was also removed. I gained a lot of weight, 18 kg from my previous weight. There is a strong distortion of the spine towards the healthy arm and chest. On this side the ribs protrude directly, and on the opposite side they seem to be inside. What to do and which specialist to contact? Thank you! ANSWER: Hello! If the ribs are just sticking out, then you don’t need to do anything, it’s just a life situation. If there is discomfort and pain, then you need to contact a neurologist to treat the pain syndrome, and the best way is to contact a reconstructive surgeon for breast reconstruction to restore balance and equal volumes of the glands.
the swelling went down, a lump was found next to the stitch
QUESTION: A month passed after the mastectomy and a week later my swelling went down, and I found a lump next to the suture. Chemistry will be this week. ANSWER: What did you want to know? Go through chemotherapy, and regarding changes in the area of the wound, contact your attending physician, and he will be able to advise you and give you an adequate answer.
Mastectomy + plastic surgery and coronavirus
QUESTION: Good afternoon, Vitaly Alexandrovich! Due to coronavirus and quarantine, are elective surgeries cancelled? On 03/25/20 I had a commission on breast cancer on Berezovaya Alley. The verdict is mastectomy + plastic surgery, they will first call you for a consultation with a plastic surgeon, and you are told to wait for the call. My question is motivated by events in the country, news changes every day. Sorry that the question may be in the wrong place. ANSWER: Hello! Surgeries haven't been canceled yet, but hospitalization rates have slowed. There is a line and there will be a line, so expect to be called to see a plastic surgeon. Perhaps it will be me. I return from vacation on 04/01/2020.
Radical mastectomy according to Madden and postoperative changes
QUESTION: Vitaly Alexandrovich, good evening! I am 49 years old and had a Madden mastectomy on January 28th. The study revealed invasive ductal breast cancer of moderate malignancy. No tumor elements were found in the nipple and axillary lymph nodes. Tamoxifen was prescribed. 2 months have passed in the axillary area, discomfort, numbness, sensation of a lump and a tourniquet. It’s as if there’s a tourniquet stretching from the elbow to the armpit. Please tell me, can such sensations exist and how can this condition be alleviated? I was in a rehabilitation center, they told me to continue doing a set of exercises, they recommended pressotherapy (but there was no improvement after it). ANSWER: Hello! The changes you listed are characteristic of postoperative changes, and now, after removal of the axillary tissue, the sensitivity of this area is restored, all the symptoms you listed above appear, this can last up to a year. Unfortunately, nothing can be done about this, it will continue and no procedures will remove this effect of pain and sensitivity. It takes time to pass. Good luck to you.
Drainage
QUESTION: After removal of the lymph nodes under the armpit, 2 weeks have passed, the drainage has stopped flowing and is twitching at the junction of the skin and the tube. What to do? ANSWER: Hello! Contact your surgeon because it has most likely stopped working and the drain needs to be removed. Any questions related to the operation should be discussed with the surgeon.
How long can I walk with stitches?
QUESTION: The mother underwent surgery to remove the mammary gland on March 19, and was discharged home on April 10 with stitches. How long can I walk with stitches? ANSWER: Hello! You can walk around with stitches for a long time and nothing will happen. During a mastectomy, sometimes they even have to walk for up to 2 months with stitches. Contact your surgeon and he will remove the stitches.
the seam turned red after 2 months
QUESTION: Good evening! My mother had a mastectomy of her left breast 2 months ago, now the stitch has turned red, is this normal? ANSWER: Hello! It’s so hard to say what it’s about, sometimes this is the norm. You can contact the doctor who operated on you or the oncologist at your place of residence, and they will answer your question about the red stitch. A suture has stages of maturation and sometimes redness of the suture is a common maturation stage of suture healing.
Skin sparing mastectomy
QUESTION: Vitaly Alexandrovich, good afternoon. Tell me, if breast reconstruction is planned a year after a mastectomy, it is possible to have a skin-sparing mastectomy. Or is it better without preserving the skin? ANSWER: Hello! If it is possible to perform a skin-sparing mastectomy, then for reconstruction it is better to preserve as much skin as possible, ask your surgeon and say that you will be doing breast reconstruction. As far as I understand, we communicated via WhatsApp on this issue.
I've been feeling nauseous for 5 days after surgery.
QUESTION: Hello doctor, I had a mastectomy of both glands with removal of the axillary lymph nodes on the right. After the operation I have been feeling sick for 5 days. What could it be? ANSWER: Hello! This could be anything: from the effects of anesthesia to other global progression problems. It’s better to discuss this issue with the surgeon, since you are still in the hospital and only 5 days have passed.
Driving a car after installing the expander
QUESTION: Hello. On 07/02/20, a mastectomy of the left breast was performed with the simultaneous installation of an expander. Is it possible to drive a personal car? ANSWER: Hello! You can drive a car, especially if the car has an automatic transmission.
Can a healthy breast hurt during chemotherapy?
QUESTION: Good afternoon, Vitaly Alexandrovich! Breast cancer 2B, we had 4 courses of red chemotherapy, a mastectomy according to Madeleine, and the last 4th course of white chemotherapy remained. Unoperated breast pain periodically. They looked at the ultrasound and everything seemed to be fine. Can a healthy breast hurt during chemotherapy? ANSWER: Hello! Of course it can. This may also be associated with the spine; during chemotherapy, bones and vertebrae sometimes hurt, which can affect the intercostal nerves, causing pain in the healthy chest.
How did the tumor affect so many nodes a week before surgery?
QUESTION: Good afternoon! Thank you for your answers 07/22/2020 left radical mastectomy was T2N0M0 G2, became T2N2aM0 IIIa Luminal B. G3 invasive carcinoma with vascular invasion. 15 lymph nodes were removed, 8 were affected by mts. Tumor IHC hormone-dependent er 100%, pr 100%, her2 +1, ki-20-25%. On examination, the lymph nodes were not palpable. How did the tumor affect so many nodes a week before surgery? They prescribed 4 courses of AC chemotherapy, 4 courses of taxane chemotherapy, and tomoxifen for 5 years. Ovarian suppression. I completed the first course of chemotherapy, platelets began to increase; they were 327 * 10^9l and became 507. I have a question: why are platelets increasing? And was the treatment prescribed to me correctly? ANSWER: Hello! I completely agree with the treatment. Platelets may increase because there is intoxication due to chemotherapy and there is not enough water in the body, drink more water. It is necessary to replenish the volume of fluid. Micrometastases may not be visible on ultrasound and other examination methods and therefore the stage was increased after histological examination
sick leave for mastectomy
QUESTION: Hello. In July 2020, a mastectomy was performed with removal of the axillary nodes. Histology - invasive tubular carcinoma G1 WITHOUT mts in the lymph nodes. Conclusion in the extract: cr of the right breast, stage 1A (T1bN0M0) VNK. IHC ER overall indicator 8. PR overall indicator 8. HER2NEU reaction negative. KI67 expression in 30-32% of tumor cells. Hormone therapy was prescribed. Triptorelin 3.75 mg (diferelin is available at the pharmacy) and tamoxifen 20 mg. At first my arm hurt a lot when I lifted it up. Now the pain is gone, but it’s difficult to do anything with your hand in a vertical position. The feeling is that she is not mine, as if she will fall, I want to constantly support her. If you sit with your elbows on the back of a sofa or chair and at the same time relax your back and shoulders, that is, slightly slouched, then after a while you will experience severe pain in your shoulder and forearm. It goes away when you straighten your back or stand up. Plus, your hand gets very tired when working at the computer. My questions. 1. Are such feelings normal in my situation? 2. How long can sick leave last in my situation? My doctor closed it before two months after the operation. Of course, I'm not a doctor, but I think it's too early. How to work with such a hand? I heard that sick leave can last up to 4 months, even if chemotherapy is not prescribed. Tell me, do I have the right to resume postoperative sick leave in order to further “heal” my arm? Thank you. ANSWER: Hello! These are typical changes after breast removal. But not everyone experiences such changes. Sick leave usually ends after 15 days, maximum 21 days after surgery, unless there is chemotherapy, in this case there is no chemotherapy. Up to 4 months of sick leave if you are just continuing chemotherapy treatment. In general, this is at the discretion of the attending physician. If you have complaints and problems, then you can go to a rehabilitation center and they can give you a sick leave, but only in the case of any ongoing treatment. This is a common situation.
recurrent pain after mastectomy
QUESTION: Good evening. 10 days after breast removal surgery. They were discharged home. I can’t sleep and have periodic pain, especially at night. Please advise what painkillers and sleep medications I can take? Also the question is, is it true that after chemotherapy and radiation it heals more slowly? ANSWER: Hello! Healing as usual. It is incorrect to prescribe treatment over the Internet. There can be various reasons for pain and insomnia. As for pain, perhaps a seroma has accumulated there and you need to be examined by a surgeon. Contact your healthcare provider.
1-50 51-71
Ask a Question
CATEGORIES
| Make an appointment [12] |
| Sign up for a consultation online [10] |
| Reviews about the work [6] |
| Internship of Skvortsova V.A. in the USA, MD Anderson Cancer Center [2] |
| Quota for breast reconstruction [17] Reconstruction of the mammary gland (breast) after mastectomy according to quota |
| Breast cancer [1388] All about breast cancer: diagnosis, treatment, breast restoration and reconstruction. |
| Diagnosis of breast cancer [112] |
| Breast diseases [126] |
| Mammography [25] |
| Ultrasound of the mammary glands (breasts) [104] |
| Computed tomography [36] |
| Scintigraphy (osteoscintigraphy) [20] |
| Cytological examination of breast cancer [12] |
| Biopsy and histological examination of breast cancer [46] |
| Immunohistochemical study of breast cancer [224] Immunohistochemical study |
| Her2neu [47] |
| her 2 [14] |
| ER and PR [11] |
| ki67 [63] |
| Surgical treatment of breast cancer [57] |
| Mastectomy [71] |
| Organ-preserving operations [29] |
| Preventive mastectomy [9] Preventive mastectomy |
| Breast reconstruction according to quota [46] What is included in breast reconstruction according to quota, breast correction after reconstruction, lipofilling |
| Breast reconstruction consultation [29] |
| Breast reconstruction (breast surgery) [178] Breast reconstruction |
| Breast reconstruction [109] |
| Reconstruction of the nipple and areola [9] |
| Breast lipofilling [21] |
| Mammoplasty (breast augmentation) [1] |
| Breast removal [3] |
| Chemotherapy for breast cancer [178] |
| Side effects of chemotherapy [26] |
| Taxanes (paclitaxel, docetaxel) [19] Taxanes (paclitaxel, docetaxel) |
| Paclitaxel [6] |
| Zoledronic acid [5] |
| Targeted therapy [54] |
| Herceptin [14] |
| Antihormonal endocrine therapy [209] Treatment of hormone-dependent breast cancer |
| Tamoxifen [141] Tamoxifen |
| Radiation therapy [97] Radiation therapy |
| IORT [10] Intraoperative radiotherapy |
| Cancer in situ [18] |
| Treatment of breast cancer [150] |
| Luminal A breast cancer [57] |
| Luminal In breast cancer [41] |
| Luminal In her positive breast cancer [28] |
| Her2neu positive breast cancer [17] |
| Triple negative breast cancer [65] |
| Breast cancer prognosis [20] |
| Treatment of breast cancer [35] |
| Treatment of stage 1 breast cancer [31] |
| Treatment of stage 2 breast cancer [24] |
| Treatment of stage 3 breast cancer [31] |
| Treatment of stage 4 breast cancer [41] |
| Breast cancer recurrence [9] |
| Monitoring the effectiveness of breast cancer treatment [10] |
| Medicines [32] |
| Vitamins [8] |
| Lymphorrhea, lymphostasis, lymphedema [64] Lymphostasis and lymphorrhea |
| Immunomodulators for cancer [4] |
| Keloid scar [1] Keloid scar |
| Ovariectomy for breast cancer [9] Ovariectomy |
| BRCA1, BRCA2 [6] |
| Tumor markers [38] |
| Mastopathy [4] |
| Fibroadenoma [28] Fibroadenoma |
| Breast cyst [15] |
| Injuries to the mammary gland (chest) [5] |
| Follow-up after breast cancer treatment [17] |
| Life after breast cancer treatment [117] |
| Myths and truths about breast cancer [31] |
| After breast cancer surgery [23] |
| Rehabilitation after breast cancer [12] |
| Miscellaneous [65] |
| Pregnancy and childbirth after breast cancer [1] |
Beneficial physical activity
Rules for caring for your health:
1. Swimming. Water soothes, has a gentle massaging effect, and the hand recovers faster. Lymph outflow is normalized. The swelling subsides.
2. Exercise. Simple to do but very effective. They will easily become a daily habit.
- “Combing your hair” Place your elbow on the edge of your bedside table. Keep your head straight. Start by combing one half of your head, then gradually move to the other. Don't get overwhelmed, but be persistent;
- “Ball” Clenching and unclenching the hand. Use a rubber ball or other object, squeezing it in your palm;
- “Drying your back” Using a towel or similar object, make gentle movements that simulate drying your back. Repeat on both sides.
3. Wearing a compression sleeve. It is necessary to prevent the occurrence of edema and the threat of lymphedema. Therefore, it needs to be worn under load: work in the country, household chores, flights or a long road. If you couldn’t put on a sleeve during physical activity, be sure to put it on afterwards. Agree that it is better to wear a prophylactic sleeve during exercise than to constantly wear a therapeutic compression sleeve if lymphedema begins to develop.
Types of reconstructive breast surgery
Breast reconstruction can be performed immediately after a mastectomy or after a certain period of time. There are many types of plastic surgery to restore female breasts. Fundamentally, all methods are divided into three large groups:
- Own tissue is used (moving muscle flaps from the back and abdomen, microvascular anastomoses).
- Artificial implants (prostheses) are used.
- Combined option.
In order for breast reconstruction to proceed without complications and give a good result, the surgeon takes into account a number of factors (anatomical features of the structure of the female body, the age of the patient, the presence of concomitant pathology, etc.). The optimal plastic surgery option is selected for each woman. [3], (paragraphs: 3-8)
Complications
There are a number of unpleasant consequences of the operation, about which the doctor must warn the patient in advance. The most common are:
- seam divergence;
- deformation of the nipple areola due to incorrect markings by the doctor before surgery;
- sagging breasts due to large volume;
- tissue infection and inflammation (the body may not accept a foreign element);
- scar formation;
- impaired blood circulation if the nipple is poorly implanted;
- loss of sensitivity (restores after a year).
1) general surgical (skin sensitivity disorders, seroma, hematoma, wound suppuration, formation of hypertrophic or keloid scars);
2) specific complications characteristic only of this type of operation (fibrous capsular contracture, as well as rupture, dystopia and deflation of the prosthesis).
The incidence of complications is given below based on an analysis of the results of 304 breast replacement operations performed at the Center for Plastic and Reconstructive Surgery in 271 patients aged 17 to 57 years from 1992 to 1997.
Sensory disturbances. Impaired sensitivity of the nipple-areolar complex is quite common (up to 21%) and can manifest itself in the form of anesthesia, hypoesthesia and even hyperpathia. The reason for this is complete or partial damage to the anterolateral and/or anteromedial branches of the fourth intercostal nerve.
DETAILS: Rehabilitation after hip replacement in the postoperative period
Seroma occurs in approximately 1% of cases. The reasons for its occurrence may depend on both the surgeon and the patient. Thus, a seroma can form when the surgeon creates an unreasonably large cavity for the implant and there is no drainage. An increase in the exudative reaction in the wound may be a consequence of the patient’s violation of the postoperative regimen, early physical activity, refusal of sufficiently long (up to six weeks) bandaging with an elastic bandage and wearing a bra.
Hematoma. The development of postoperative hematoma (1% of cases) can lead to suppuration of the tissue around the implant and is one of the factors contributing to the formation of capsular contracture. A significant role in the prevention of this complication is played by careful stopping of bleeding and drainage of formed cavities with normal indicators of the blood coagulation system.
The suppuration of the wound around the prosthesis was 0.6%. It requires removal of the prosthesis and, as a rule, leads to an unsatisfactory result. Preventive measures include strict adherence to asepsis, careful stopping of bleeding, washing of formed cavities with an antiseptic and antibiotic solution, as well as a single preoperative administration of broad-spectrum antibiotics in prophylactic doses.
Hypertrophic and keloid scars. The formation of hypertrophic and keloid scars in most cases is associated with individual characteristics of the connective tissue reaction to injury. Therefore, the likelihood of developing such a complication should always be discussed when talking with the patient.
Bedsore. Errors in surgical technique during breast replacement can lead to pressure sores from the pressure of the prosthesis on the tissue of the lower pole of the gland. In particular, when placing an implant directly under the breast tissue, the surgeon must create a cavity exclusively between the fascial sheath of the mammary gland and the fascia proper of the pectoralis major muscle. Therefore, careful layer-by-layer closure of the wound with suturing of the fascia is a prerequisite when performing this operation.
Dystopia of the prosthesis. In total, there are five types of prosthetic dystopia: location too high, too low, lateral displacement of the prosthesis outward or inward, as well as rotational dystopia, characteristic of anatomically shaped implants when their vertical axis is displaced (Fig. 37.2.4).
The causes of implant dystopia are errors in planning the formation of a cavity for prostheses, as well as insufficient consideration of the anatomical features of the structure of the chest.
Postoperative deformity. The formation of a wave-like deformation along the upper inner edge of an anatomically shaped prosthesis occurs in up to 10% of cases 2-3 months after surgery in patients with a thin subcutaneous fat layer and well-developed pectoralis major muscles.
The presumable mechanism for the development of this phenomenon is that after installation of the prosthesis, the area of fixation of breast tissue to the chest is significantly reduced. The downward displacement of the gland tissue under the influence of gravity leads to stretching of the thin subcutaneous fat layer covering the upper and lateral edges of the prosthesis.
Hourglass deformation of the endoprosthesis or its displacement in the cranial direction can occur when the implant is placed under the pectoralis major muscle during its contraction. This occurs in cases where during the operation the surgeon does not cut off the lower portion of the muscle from its attachment to the ribs and sternum.
Prosthesis rupture most often occurs when performing a closed capsulotomy, as well as due to injuries and without clearly established causes (only about 10%). This most often occurs when using prostheses with a very thin shell or an incompetent valve.
Leakage of the prosthesis (deflation) This complication is typical for infillable prostheses or for prostheses with a double shell. Loss of volume of the prosthesis can occur due to the diffusion of isotonic sodium chloride solution through its shell or through the injection port of the implant.
After endoprosthetics, women experience pain when moving or mechanical impact on the mammary glands, decreased sensitivity of some areas of the skin, swelling and slight asymmetry. As a rule, these sensations pass as the tissues are restored and the body gets used to the implants. In some cases, the following complications are observed:
- Increased volume and firming of the breasts. It appears no less than six months after surgery due to compression of scar tissue around the implant. The complication does not pose a threat to health, but the aesthetic effect deteriorates significantly, and sometimes surgical intervention is required for correction. The risk of developing this condition can be reduced by choosing new generation implants with a textured surface.
- Bleeding or tissue infection. If in the postoperative period there is bleeding from the incision sites, discharge from the nipples, fever or deterioration in general condition, you should immediately consult a doctor.
- Seroma and hematoma. In the surgical area, lumps that rise above the skin and are filled with blood or serous fluid may appear. This is a fairly rare complication that can be treated with conservative methods.
Contrary to popular belief, endoprosthetics and installation of breast implants are not capable of triggering the growth of malignant tumors. Medicine knows cases of the development of benign formations, but the percentage of such complications is extremely small.
Endoprosthesis replacement is a practically safe operation that can significantly improve the appearance of the breast. If you pay enough attention to choosing a plastic surgeon and follow all medical recommendations, the result of the surgical intervention will please the woman throughout her life.
Recovery period
After plastic surgery, the woman is transferred to an inpatient department under constant medical supervision. Typically, hospital stay is from 5 to 7 days. All this time, the transplanted tissues are monitored by modern sensors that measure the slightest changes in temperature and tissue oxygenation. Before discharge, the doctor conducts a follow-up examination and, in the absence of any complications, gives all the necessary recommendations for the further postoperative period.
During the week after plastic surgery, a woman may experience pain. In order to relieve symptoms, the doctor prescribes painkillers. A week after discharge, you must visit the clinic, where the surgeon will assess the speed of wound healing and set a date for suture removal. Full recovery of the body will occur after 2-3 months. After this, you can begin the final stage of reconstruction - recreating the shape of the nipple using surrounding tissue. The nipple areola is applied using a tattoo technique.
DIEP flap reconstruction technique
The DIEP flap (Diep inferior epigastric perforator) contains only skin and fatty tissue. The abdominal area also serves as a donor for the DIEP flap. The DIEP flap is moved freely, without a vascular pedicle. Thus, its subsequent connection with the tissues in the chest area is carried out microsurgically.
Advantages of DIEP flap reconstruction:
— No allergic reactions; — The result is as natural as in the method described above; — Additional abdominoplasty; “The risk of weakening the abdominal muscles and causing a hernia is still significantly less than with TRAM flap reconstruction.
Disadvantages of DIEP flap reconstruction:
— Scar in the abdomen; — There must be a sufficient amount of fatty tissue to serve as a donor; — The operation is also quite traumatic. — After microsurgical suturing of blood vessels, there is a slight risk that they will not heal well enough.
Breast reconstruction with LAT flap
LAT (Latissimus dorsi) The technique involves the use of donor tissue from the back, namely the latissimus dorsi muscle. Donor tissue is collected with nutrition, that is, on a vascular pedicle. The tissue moves through a subcutaneous tunnel formed by the surgeon.
Advantages of LAT flap reconstruction:
— Suitable for thin patients or for those who have previously had surgery in the abdominal area; — The large abdominal muscle is not damaged; — The donor site receives nutrition.
Disadvantages of LAT flap reconstruction:
— A scar remains on the back; — Often there is not enough adipose tissue in this area, so additional installation of an implant is necessary; - Possible weakening of the shoulder or back muscles.