Puva therapy is a fairly effective method of treating psoriasis. This is a method of irradiating affected areas of the skin, known since 1978. So, if you have been suffering from this disease for a long time and do not know how to help yourself, try puva therapy.
Today, when the world is oversaturated with all sorts of artificial substances, this method of combating various skin diseases is acceptable. And it’s not surprising, because puva therapy is the interaction of ultraviolet rays and healing substances of plant origin.
The essence of using Puva therapy
PUVA (Puva) - the name of this physiotherapeutic procedure, arose from the words Psoralens and UltraViolet A. It was invented more than forty years ago and is now actively used not only for the treatment of psoriasis, but also mycosis fungoides, atopic dermatitis, vitiligo and other dermatological disorders. Indeed, in 80-85% of cases, treatment with puva therapy helps.
Irradiation is carried out in medical institutions (clinic, dispensary or special centers), regardless of the patient’s work schedule or employment. You do not need to go to the hospital for the procedure; you just need to come to see the doctor at the appointed time.
The essence of using Puva therapy involves taking photosensitizing drugs followed by exposure to ultraviolet light on problem areas of the skin. The initial procedure only takes a few minutes. In subsequent “ultra-attacks”, at the discretion of the attending physician, the time may be slightly increased.
It happens that in order to achieve a more effective effect, the patient is prescribed a combined technique. That is, the whole body is irradiated, adding several sessions to the most affected areas. The dose of light therapy is selected for each patient, it depends on:
- the type of skin that will be susceptible to ultraviolet radiation;
- the result of increased irradiation of the most affected areas of the skin (from 2 cm or more). If 2-4 days after Puva therapy does not cause a strong reaction (redness or pigmentation), at the discretion of the doctor, the dose for treatment may be reduced by half.
And yet, after the end of light therapy and oral administration of the drug Psoralen, the patient is recommended to wear sunglasses for a day or two, which will help prevent the development of cataracts.
Indications and contraindications
Many patients have a question about what puva therapy is and in what cases is it used? Indications:
- Most often, this technique is used to treat plaque psoriasis of the feet and palms. Puva therapy in practice shows good results in the treatment of this disease. Treatment is aimed at blocking the proliferation of cells that are the source of the skin rash. As a result, the plaques stop developing and after a while disappear completely.
- Fungal mycosis and atopic dermatitis.
- Vitiligo. The therapy is also used in patients whose skin damage reaches 25-30%.
Puva therapy for psoriasis is not carried out at home. The entire treatment process is performed only in a medical facility under the supervision of the attending physician. The drugs are prescribed locally or orally, after 2-3 hours the patient must undergo irradiation with a UV lamp. The course of treatment is determined by the doctor; it ranges from approximately 10 to 30 sessions.
But complex and local photochemotherapy has contraindications:
- individual intolerance to the active substance – psoralen;
- the presence of any malignant neoplasms;
- lupus erythematosus;
- albinism;
- pregnancy and lactation;
- xeroderma psoriazepigmentosa.
If the patient has fair skin and has any skin diseases other than the main diagnosis, for example, acne, then the doctor may prohibit the use of this method. Puva therapy is prescribed with special caution for cataracts, uremia and kidney diseases. It is also recommended to look for an alternative treatment method for patients with low immunity, diseases of the cardiovascular system and varicose veins.
Visible effect after a course of Puva therapy
How it works
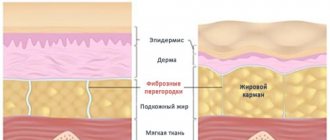
When irradiated with ultraviolet light, it reduces inflammation at the site of the lesion, has an antibacterial and immunomodulatory effect and promotes the regeneration of damaged epidermal cells.
But ultraviolet rays themselves are not that effective. Therefore, they are combined with oral medication, which only increases the effectiveness of long-wave UV rays.
Puva therapy for the treatment of psoriasis mainly uses herbal preparations, known medically as psoralens and methoxypsoralens. They are well tolerated by patients, absorbed and excreted within 12-24 hours.
PUVA therapy increases skin sensitivity and resistance to the formation of new psoriatic rashes. This is achieved by the fact that photosensitizing drugs inhibit DNA synthesis in epidermal cells and block their mitotic division.
Irradiation equipment
Puva therapy for psoriasis involves the use of certain settings. Various PUVA devices are used to carry out a complex of photochemotherapeutic procedures. They provide the necessary long-wave ultraviolet radiation.
Modern radiation rooms are mainly equipped with booths or screens with built-in fluorescent lamps that affect the entire body. There are also devices for topical use, when specific areas need to be exposed to UV radiation, for example, the palm or both, the inside of the foot, elbow, knee or scalp.
Principle of photochemotherapy
The procedure is based on the action of photosensitizers, which increase the sensitivity of skin cells to ultraviolet radiation and help clear dermatoses. Without the required dose of radiation, psoralens are ineffective . Once in the body, they bind to the DNA of epithelial cells and suppress the synthesis of proteins and nucleic acids, blocking further division of pathogens that form skin rashes.
Based on their origin, there are natural (“Amminofurin”) and synthetic (“Trimethylpsoralen”, “Methoxalen”) photosensitizers. Typically, these substances are well processed by the liver and excreted from the body within 24 hours.
PUVA therapy sessions are carried out on an outpatient basis and are compatible with work or study. 2-3 hours before each procedure, the patient must take a medicine with psoralen, which is better absorbed with milk or low-fat food. The initial exposure to ultraviolet radiation on the affected skin does not exceed a few minutes, then the duration of the sessions gradually increases. As a precaution, after irradiation it is recommended to wear sunglasses for 24 hours to avoid damage to the retina and the development of cataracts.
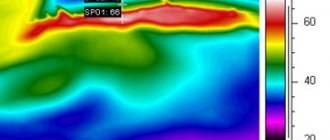
The determining factor for determining the duration of one session is skin type. Additionally, areas of the epidermis not exceeding 2 cm are irradiated, with a gradual increase in dosage. The skin reaction is recorded after 2-3 days. To determine the required amount of ultraviolet radiation, the part of the epithelium with the lowest levels of inflammation/irritation is selected. In this case, the initial volume of UV rays is reduced by 2 times.
Most used treatments
The use of puva therapy involves only three types:
- systemic (general) - the most applicable procedure, which involves taking tablets followed (after 2-3.5 hours) by UV irradiation;
- local or topical - the effect is only on the affected area of the skin and involves the application of a photosensitizing cream or emulsion with further dosed exposure to ultraviolet radiation;
- puva baths are also a type of therapy and involve taking a bath with psoralen, which must first be dissolved in water.
Most popular: The benefits of organic silicon for beauty and health
Photosensitizers, that is, psoralens, are also divided into groups. To treat skin diseases, in particular psoriasis, the following types are used:
- natural - those made from plant materials, for example, citrus fruits, umbrella or legume plants. For example, the domestic drug is Ammifurin. Or Methoxsalen, an imported medicine widely used for puva treatment;
- synthetic - chemical drugs such as Trimethylpsoralen, which are also used for other skin diseases (vitiligo or dermatitis). But remember, they are used only as prescribed by a doctor, who calculates the dose depending on the patient’s body weight and recommends taking them internally or externally.
Progress of the procedure
Phototherapy is carried out in a hospital setting, a dispensary, special institutions, but without a hospital. Before the procedure, psoralens are consumed with milk or lean food. After a few hours, the patient must go into a booth or stand behind a screen to receive the required dose of ultraviolet radiation.
Manipulations take place in a standing and lying position; patients place the scalp, affected surfaces of the palms and soles under a fluorescent lamp. In this case, local processing is used using portable devices.
The first session lasts no longer than 2-3 minutes, after which the duration of each subsequent procedure increases. The radiation dose is affected by the patient's skin type. In advanced stages of psoriasis, the entire body is treated. However, during the first manipulation it is necessary to irradiate a small area of the epithelium in order to then evaluate the effectiveness of therapy after a few days.
After the treatment process, it is important to wear sunglasses for 24 hours to protect against cataracts. Local PUVA therapy is increasingly used, since with a local effect on the affected area, the maximum result is achieved.
To achieve stable remission, it is necessary to carry out 10-30 manipulations with a one-day interval between sessions. In the future, maintenance treatment is prescribed, and the radiation dose is gradually reduced.
If baths are used to treat the epithelium with psoralens, the subsequent procedure lasts about 15 minutes. This technique is often used in European institutions. Baths are used if patients have adverse reactions to the internal intake of photosensitizing substances.
This method is also prescribed if the patient is affected by squamous cell carcinoma or palmoplantar psoriasis. PUVA baths are well tolerated and provide excellent results for severe forms of lichen planus. The full course consists of 15-25 sessions. If the palms or feet are affected, at least 30 manipulations are performed.
The Superiority of PUVA Therapy
People who have undergone photochemotherapy to treat psoriatic rashes report:
- Quick effect - suppression of the formation of new rashes and regression of existing manifestations is already noticeable in the 3rd or 5th procedure;
- High quality - patients experience complete cleansing of problem areas of the skin, while all others experience significant improvement;
- Puva therapy has excellent tolerability;
- Reduction of relapses - after PUVA sessions, long-term remission is maintained (from six months to several years);
- Lack of addiction, which makes the therapy method more effective;
- Outpatient treatment without interruption from work or study (for an hour, you can always leave for another);
- Aesthetics - after completing a course of photochemotherapy, a beautiful, uniform tan remains;
- Practicality - maintenance radiation sessions can always be carried out.
What is the essence of the procedure
Puva therapy for the treatment of psoriasis is used exclusively in outpatient settings , such as dispensaries, clinics, and specialized centers for the treatment of psoriasis. At the same time, there is no separation from work or study.
Photosensitizing agents are taken orally with low-fat foods or milk, and after a certain time, those areas of the skin that are affected are exposed to ultraviolet rays. The first procedure is carried out for several minutes, and in subsequent sessions the irradiation time is increased.
If necessary, two treatment methods are combined: local irradiation and general exposure. The required dose for irradiation is carried out using two methods:
- According to skin type;
- Gradually increasing the dosage of irradiation of skin areas with a diameter of 2 centimeters. The result is checked after 72 hours. When treating psoriasis, experts prescribe half the dose that caused the slightest pigmentation or redness.
After photochemotherapy with oral psoralen for 24 hours, the patient is required to wear specialized sunglasses. This procedure is necessary to prevent cataracts.
The best way to treat Puva - therapy for psoriasis - is local. It is most effective because it acts directly on the affected area of the skin .
Disadvantages of the technique
There are several “disadvantages”, which are:
multiple visits to the Puva office - the disease cannot be eradicated in one procedure; negative side effects - the skin is too sensitive and tender, it can become very red. Patients taking photosensitizing drugs by mouth may experience:
- nausea with vomiting;
- refusal to eat;
- abdominal discomfort;
- severe itching of the skin;
- allergic rashes;
- dizziness and severe pain;
- insomnia;
- signs of hypotension;
- Puva therapy provokes depression.
Most of these unpleasant side symptoms occur in only 10-15% of people treated with Puva therapy. Again, depending on the characteristics of the body. Such side effects do not last long and do not require any additional treatment at all, as they disappear on their own. And to alleviate such conditions, doctors recommend:
- drink psoralens with milk or some other food;
- during puwa sessions, switch to fractional meals - often and a little at a time;
- divide photosensitizing tablets into several doses;
- for severe nausea, use antiemetic drugs;
- reduce the dose of herbal medicine and accordingly increase the amount of ultraviolet irradiation.
Negative reactions can also occur with external use of psoralens. After applying the cream or emulsion, the following are occasionally observed:
- excessive dry skin;
- terrible itching, burning;
- allergies in the form of dermatitis.
Similar phenomena also occur in a small number of people - only 1-20%, 2-3 days after a puva session. To eliminate them, ointments, gels and creams with a softening effect are used.
Manifestation of overdose
If large, severely itchy erythema with blisters and unbearable pain appear on the body after the first or subsequent procedures, then this indicates an incorrect prescription. That is, either the doctor chose the wrong dosage of the medicine and radiation, or the technique is generally contraindicated for you.
Most Popular: Selecting the Best Drugstore Creams for Dry Skin
In this case, undesirable consequences include:
- increased pigmentation - pronounced spots;
- burns;
- keratitis;
- increased burning and itching;
- premature aging of the skin (manifested by the appearance of wrinkles, sagging);
- conjunctivitis or cataracts;
- oncological manifestations - skin cancer in the form of carcinoma or melanoma.
Fortunately, these are very rare manifestations, to avoid which, all patients undergoing Puva therapy are required to undergo additional annual examination. To prevent cancer, all the most vulnerable areas are covered with protective devices, unless there are psoriatic rashes there.
How the method works
Psoralens themselves do not have any effect on the skin. Once they enter the body, their effect begins only after they are exposed to ultraviolet rays.
After psoralens are activated, they begin to interact with the DNA of epidermal cells. Photosensitization selectively leads to suppression of DNA synthesis in the epidermis , but no corresponding suppression of cell functions occurs. After 1.5 hours after taking psoralen, photons of UV rays that are absorbed begin to provoke photochemical binding of DNA cells by the formation of cyclic bonds between the pyrimidine bases of DNA cells and the photosensitizer. The mechanism of the main action of such drugs is the formation of “DNA-photosensitizer” cross compounds, which are capable of reducing the level of epidermal DNA synthesis.
Psoralen molecules are capable of stimulating the formation of active oxygen, which can activate the metabolism of arachidonic acid and cause damage to the membranes of epidermal cells. These molecules contribute to the initiation of chemical reactions that lead to the death of lymphocytes and keratocytes and suppress the processes of pathological keratinization .
It has long been known that ultraviolet irradiation in the presence of psoriasis has a positive effect on the body. It can have an immunomodulating, bactericidal, anti-inflammatory effect, and helps stimulate the synthesis of melanin by skin cells. To increase the effectiveness of ultraviolet radiation during puva therapy, it is necessary to simultaneously use long-wave ultraviolet rays and drugs that have photosensitizing properties.
Contraindications
The prohibition for treatment with the RUVA technique is the presence of the following conditions:
- hypersensitivity to psoralens and UV rays;
- hyperreaction to light (observed in some diseases, such as lupus);
- malignant skin manifestations;
- ophthalmological defects and pregnancy.
Puva therapy is not prescribed to patients with psoriasis with severe cardiovascular diseases, when the patient cannot stand in a UV cabin for a long time.
PUVA dosing
The frequency of sessions is also assigned based on the characteristics of the person. Basically, the course includes 10 or in severe cases 30 procedures, which are important to attend 3-4 times a week, that is, every other day. At the discretion of the doctor, preventive phytochemical treatment may additionally be used, when the dosage of medications and visits is gradually reduced.
Contraindications for carrying out
PUVA therapy, like any other procedure, has a number of contraindications:
- presence of allergies (an allergic reaction to the use of photosensitizers may occur);
- increased sensitivity to UV rays;
- pathologies due to increased photosensitivity include porphyria, albinism, etc.
- malignant melanoma;
- aphakia;
- pregnancy;
- lactation;
- lupus erythematosus;
- children's age (in this case, procedures are carried out only after consultation with a specialist).
People with fair skin are advised to exercise caution during treatment. As well as those with reduced immunity, kidney failure, cataracts, uremia and liver diseases were diagnosed.
Herbal bathing
It is worth mentioning the use of puva baths - an advanced treatment method for psoriasis and many other dermatological diseases in leading European clinics. There, the use of photochemotherapy in water is an effective method, which consists of a 15-minute immersion in psoralents dissolved in water, followed by long-wave ultraviolet radiation.
In our country, herbal bathing has been practiced for about 10 years. This method is prescribed to patients whose body does not accept the use of photosensitizing tablets. The technique is actively used to treat children with psoriasis and under 15 years of age. Puva baths are well tolerated by patients and do not cause unwanted side effects. In addition, they can also be used locally - immerse the foot or elbow in a water-psoral solution.
Typically, doctors prescribe 15-20 sessions for therapeutic effect. In advanced cases, their number is increased to 30-40.
PUVA at home
Photochemotherapy for simple and minor skin lesions can be carried out at home. There are special ultraviolet irradiators for this purpose. They are easy to operate and do not require much effort. The only thing is that you still have to go to the doctor, as he will be able to prescribe the required dosage of concomitant medications. However, these procedures are best carried out under the supervision of a medical professional.
PUVA baths
Puva therapy - baths, what is it? This procedure is an improved version of photochemotherapy, when psoralen is prescribed to the patient in the form of a bath with a medicinal solution and subsequent exposure of the skin to UV rays. After baths, the maximum irradiation time is 10-20 minutes. The concentration of the solution in the bath and the residence time are determined only by the attending physician; with improvements, the residence time decreases.
In Russia, puva baths have been used for less than 10 years. This is a young procedure that has not yet become widespread in medicine. Photosensitizing drug solution Ammifurin (3%). Less commonly used is Methoxalen in capsules that are dissolved in water. This method of therapy is prescribed to patients who experience side effects when taking psoralen orally. Additionally, aromatic retinoids can be used for patients who have a history of cancer and for children under 16 years of age.
Puva baths have shown a high level of effectiveness in the treatment of psoriasis of the palms and feet. This method reduces the period of exposure to UV rays on the body, which minimizes the development of any side effects. In 95% of cases, baths are well tolerated by patients in adults and children. Baths effectively treat severe psoriasis with a large area of distribution. This is a good alternative if local or complex puva therapy causes any side effects.
Contraindications and precautions
Various side effects may occur after PUVA therapy:
- Skin itching.
- Nausea.
- The occurrence of burns on the skin.
- Vomit.
- Decreased appetite.
- Cataract.
- Depression.
- Skin hyperemia.
- Dizziness.
- Insomnia.
- Skin cancer and aging.
PUVA therapy is contraindicated in the presence of the following factors:
- Age category up to 12 years.
- Diabetes disease.
- Glaucoma or cataract.
- Hypertension of I and III degrees.
- Use of medicines containing tar.
- Blood pathologies.
- The presence of a malignant or benign neoplasm.
- Pregnancy and lactation period.
- Hypersensitivity.
- Acute and chronic diseases of the kidneys and liver.
- Increased photosensitivity.
- Endocrinopathy.
To avoid negative consequences from the procedure, experts strongly recommend:
- Use sunglasses and creams for at least 8 hours after the session.
- Do not use cosmetics containing coal tar.
- Inform medical staff in a timely manner about the presence of allergic reactions, skin and eye diseases.
- It is recommended to carry out the procedure at the same time.
- For men, it is quite important that the groin area is not exposed to ultraviolet radiation.
- Stay in the sun for a minimum amount of time for 8 hours after the procedure.
- It is not recommended to drink alcohol before the procedure.
Treatment with the drug is contraindicated for benign and malignant tumors, hypersensitivity to photosensitive drugs, and diabetes mellitus. You should not take the drug if you have severe liver or kidney diseases or increased photosensitivity. Treatment with the drug is contraindicated for children under 12 years of age, pregnant and lactating women.
Simultaneously with Methoxalen, treatment with such drugs as: Anthralin, Tar, Fluoroquinolones, Griseofulvin, Nalidixic acid, Quinolones, Sulfonamides, Tetracyclines and other photosensitizing drugs is prohibited.
Wear sunglasses before PUVA therapy to avoid damaging the retina and causing cataracts. Lubricate your face with sunscreen. Men should not expose the groin area to ultraviolet radiation to avoid impotence. For patients with skin types 1 and 2, it is better not to use more than 1-2 courses per year.
After the PUVA therapy procedure, it is advisable to moisturize the skin well with hydrating agents. They will restore the hydrolipid layer. These products can be based on Shea butter, linoleic acid, glycerin, aloe extract, allantoin.
Types of PUVA Treatments
Local therapy, when psoralens are applied to areas of the skin affected by psoriasis (or taken orally in the form of tablets and capsules), after which the skin is exposed to UV radiation.
PUVA bath. The patient lies in a bath with psoralen dissolved in water; upon emerging from such a bath, the patient is irradiated with ultraviolet rays.
Systemic therapy. A patient with psoriasis takes psoralens in tablet form. This process produces results later than the other two types of PUVA therapy and can last up to 25 sessions - 3 treatments per week.
For ultraviolet irradiation, there are booths in which fluorescent lamps work. They provide radiation of waves of the length necessary for the patient’s recovery. The booths are divided according to the position of the patient's body into standing, lying, and for irradiation of individual areas of the body.
Consequences and possible complications
After application, the consequences can appear both in the near and long term. In the early period, various negative skin reactions most often occur, for example, itching, excessive dryness of the skin, and the appearance of blisters with transparent contents. Taking photosensitizing drugs orally, in addition to these symptoms, can cause a feeling of discomfort in the stomach and nausea.
Phenomena such as:
- Koebner phenomenon;
- painful sensations on the skin;
- headaches;
- hypertrichosis;
- malaise;
- hemorrhages under the nail plates;
- the appearance of a vesicular rash.
When treated with this method, secondary pigmentation of the skin develops in those areas where irradiation was carried out. This phenomenon does not have any dangerous consequences, and after a few months the usual skin color returns.
There are also complications that are much more dangerous than the side effects described above. They develop over long courses. In particular, the risk of skin cancer becomes much higher, especially if the total number of procedures is about 260. In addition to such a serious complication as cancer, this list also includes cataracts. Photoaging also occurs faster.
But it is noted that photochemotherapy itself almost never leads to the development of either squamous cell or basal cell skin cancer. This complication is only possible if the patient himself already has a predisposition to the disease, or there are factors that accelerate its development (smoking, frequent exposure to the sun, treatment with other methods of ultraviolet exposure, etc.).
PHOTODYNAMIC THERAPY
Photodynamic therapy (PDT) uses photosensitizing chemicals to kill precancerous or cancerous cells. The main topical sensitizing agents used in practice are 5-aminolevulinic acid (ALA) and methylaminolevulinic acid (MAL) (a related but more lipophilic methyl ester of ALA that can penetrate more deeply into the target skin). Both are precursors of protoporphyrin IX (PpIX) in the heme biosynthetic pathway. The main absorption peaks for both agents fall in the blue (410-420 Nm) and red (630 Nm) light ranges. Treatment protocols for ALA typically use blue light, whereas treatment protocols for MAL use red light to activate the mixture.
PpIX accumulates predominantly in psoriatic plaques; PDT-induced T cell apoptosis may lead to a reduction in inflammatory cytokines and, in turn, an improvement in psoriasis.131, 132 Despite the theory, clinical studies have failed to find a significant benefit in treating psoriasis with ALA-PDT or mal-PDT. . In an analysis of 3 studies examining the effect of ALA-PDT in the treatment of plaque psoriasis, the efficacy estimate was calculated at 22%.80 There was also a relatively high rate of adverse effects. Another systematic review of 14 studies supported the conclusion that ALC-PDT is minimally effective with significant side effects.133
PDT has also been investigated as a treatment for nail psoriasis. In an open-label, in-hospital, left-to-right comparative study with 14 subjects, 61 psoriatic nails were treated with MAL-PDT using a pulsed dye laser (PDL) as the light source, while 60 psoriatic nails were treated with PDL alone.134 Patients received monthly treatment with Nail Psoriasis Severity Index (NAPSI) scores at baseline, after 3 months and after 6 months. Although NAPSI scores improved with both treatments, there was no significant difference in psoriatic nails treated with topical MAL plus PDL versus PDL alone. Based on the available data, the use of mal-PDT with PDL for the treatment of nail psoriasis cannot be recommended.
Recommendations for performing PDT
The strength and level of evidence of recommendations for PDT are summarized in Tables XIV and ., 133 , 134
Table XIV Strength of recommendations for PDT
| Recommendation no. | Recommendation | The Power of Recommendation |
| 5.1 | For localized psoriasis, including palmoplantar psoriasis and nail psoriasis, in adults, topical Ala-PDT and Mal-PDT are not recommended | One |
View table in HTML format
ALA, 5-Aminolevulinic acid;
MAL, methylaminolevulinic acid; PDT, photodynamic therapy. Table XV level of evidence for PDT
| Recommendation | Recommendation no. | Level of evidence | Research |
| 5.1 | I-II | , 133 , 134 |
View a table in HTML format
Reviews
Most of the reviews left by clinic visitors remain positive, since the treatment method itself has shown high effectiveness in combating even the most serious stages of the disease. As for such dangerous complications as cancer or cataracts, it is noted that with proper protection and individual selection of the duration of procedures, this can be avoided.
Based on the results of the full course, the majority of patients noted skin rashes, itching and dryness, recommending that anyone planning PUVA therapy in the future use moisturizers and antipruritics. Some people noted that the itching was almost unbearable, and severe erythema and irritation developed. However, such cases are usually associated with incorrect selection of medication dosages and duration of exposure to UV rays.
Preparation for the procedure
Before you start taking the pills included in the course of photochemotherapy, you must start using glasses. They should be worn throughout the next day after the session.
It is advisable to take a shower to remove dirt, lipid film and simply substances accumulated on the skin during the day. This should be done before applying the medicine (for local therapy) or before a PUVA bath. It is important to keep your face and hair dry. You will need to apply a product with high UV protection to your face and neck area.
Men should cover their groin area before starting the session.
Mechanism of action
The method (PUVA therapy) is based on a combination of medications and ultraviolet A radiation. At first glance, this is a rather incomprehensible procedure, but its effectiveness is undeniable.
PUVA therapy, what is it and what is its mechanism of action? The method is based on direct toxic suppression of activated lymphocytes. Psoralens are a group of drugs that, regardless of their origin (plant or synthetic), have the ability to absorb light waves. Examples of such agents are Matoxalen, Methoxypsoralen, Ammifurin, Trioxalen and others. All these agents are activated only under the influence of sunlight.
Ultraviolet treatment is carried out in medical offices equipped with solarium-type cabins. Now there are various modifications - both for irradiating individual parts of the body and for irradiating the entire surface. With the help of PUVA therapy you can get rid of psoriasis, solar urticaria, mycoses, lichen and other ailments.
Observations show that as a result of inattention to the dosage of exposure to rays, various complications arise in patients. Therefore, experts do not encourage PUVA therapy with a device at home, but despite this, manufacturers produce portable UV irradiators.