general information
The operation involves removal of the affected gland, and, if indicated, excision of axillary lymph nodes and pectoral muscles in combination with fatty tissue. The type of surgical intervention depends on the size and stage of the tumor, the presence or absence of metastases, and the type of tumor.
Important details:
- timely removal of ductal carcinoma, sarcoma, and other types of tumors reduces the risk of an extensive pathological process and the formation of distant foci with atypical cells,
- When a mutated BRCA1 gene is detected, prophylactic mastectomy, removal of mammary glands in case of a precancerous condition or a family history of cancer pathologies, is effective. After a preventive mastectomy, the risk of developing a malignant process is reduced from 90 to 34%. It is important to take into account the indications and limitations, learn about possible complications and consequences, advantages and disadvantages of the operation,
- Contacting a mammologist at an early stage of cancer pathology allows you to get by with organ-conserving surgery. In advanced cases of cancer, the active process of metastasis requires excision of the affected mammary gland,
- You should not refuse a complete radical mastectomy if the mammologist insists on this type of operation: the sooner the tumor stops its negative impact on the body, the more favorable the prognosis of therapy.
Breast removal requires highly qualified breast surgeons. A complex operation is performed under general anesthesia and lasts 3 hours or more. The duration of surgical intervention increases during reconstructive plastic therapy.
Learn about the symptoms of progesterone deficiency, as well as ways to replenish the hormone deficiency.
Instructions for using the drug Gordox for the treatment of pancreatitis of the pancreas are described on this page.
Several modern technologies are used to perform a mastectomy:
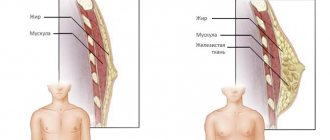
- Madden mastectomy. The surgeon removes only the affected gland; the lymph nodes and chest muscles are not affected. Indications: development of ductal carcinoma, preventive mastectomy for hereditary predisposition to cancer,
- Patey's method. During the operation, the doctor excises not only the gland with the tumor, but also the pectoralis minor muscle and lymph nodes in the armpits. Indications: confirmed breast cancer, presence of metastases,
- Halstead method. During the operation, the surgeon cuts out the affected gland, adjacent lymph nodes, pectoral muscles and fat in this area. The important thoracic nerve is not affected. Indications: extensive tumor process, there are metastases, chest muscles are affected.
To reduce the risk of depression and eliminate a severe cosmetic defect, one-stage breast plastic surgery is performed after excision of the problematic element.
What is radical mastectomy
Radical, i.e., removing entirely, completely, from the roots. The concept of mastectomy is of Greek origin - mastòs “breast” and ek tome “remove”. The term is over 100 years old.
Several types of mastectomy are practiced. Each of them is effective, they differ in the degree of trauma. Radical mastectomy is a complex operation, but sometimes it is the only one that can solve the existing problem.
There are three main types of mastectomy:
- according to Madden,
- by Patey,
- according to Halstead.
Radical mastectomy according to Madden is considered the most gentle.
Carefully! The video shows a radical mastectomy (click to open)
[collapse]
Contraindications
Resection of the affected gland for oncopathology is not performed in the following cases:
- severe brain disorders,
- renal or liver failure,
- severe forms of hypertension,
- decompensated diabetes mellitus,
- severe heart and vascular diseases,
- infectious and inflammatory processes in the body that sharply reduce immunity (temporary limitation),
- mental disorders,
- extensive tumor process, active spread of metastases, ulcers on the skin of the mammary glands.
There are also restrictions for preventive (prophylactic) mastectomy:
- presence of cardiovascular diseases, diabetes mellitus, hypertension, bronchial asthma,
- the patient is over 65 years old,
- mental disorders have been identified,
- lipomatosis of the second or third degree develops.
Preparing for surgery
The patient undergoes a medical examination:
- performing an MRI or CT scan,
- skeletal scintigraphy to detect metastases,
- biochemical and general blood test,
- x-ray of the chest area,
- Analysis of urine,
- conducting an ECG, measuring blood pressure.
Based on the results of the examination, the oncologist-mammologist selects the optimal method of breast resection and identifies possible contraindications. A week before the start of surgical treatment, you should stop taking anticoagulants and heart medications that thin your blood. In the evening you need to eat lightly; on the day of the operation it is forbidden to receive water and all types of food.
How is gland removal done?
Removal of affected mammary glands consists of several stages:
- general anesthesia,
- removal of the problematic gland, excision of fatty tissue and axillary lymph nodes,
- depending on the individual characteristics and type of pathology, the doctor leaves or removes the nipple,
- application of self-absorbing sutures or staples, wound disinfection, installation of a drainage system,
- After the operation, the mammologist sends a sample of breast tissue in the operation area for cytological examination. It is important to find out whether cancer cells remain in the problem area.
On a note! The woman stays in the clinic for 34 days, sometimes longer if there is no inflammation or other complications. To drain the accumulated fluid, the surgeon installs a drainage system. Before discharge, the patient receives recommendations for maintenance of the drainage tube system. Be sure to go to dressings and take analgesics.
Restoration options using the patient’s own tissue
Operations in which flaps of one’s own tissue are used to create breasts are more traumatic and technically more difficult. But after them the breasts look more natural.
- Using a flap from the latissimus dorsi muscle (other names: LDM flap, TDL flap). From the latissimus dorsi muscle and the skin above it, a flap is cut out on a vascular pedicle, from which the breast is formed. Since it is impossible to take a large volume of tissue from the back, they are supplemented with a silicone implant. The gland is more natural compared to simple implantation of a silicone prosthesis, but scars after the incisions are often visible on the back.
- Using a abdominal flap (TRAM flap). On the anterior abdominal wall, the volume of subcutaneous fat is usually greater than on the back, which often makes it possible not to use an implant. Moreover, when weight fluctuates, the musculocutaneous tissue taken from the abdomen increases or decreases in volume along with the rest of the subcutaneous tissue, and the breast remains symmetrical. In the traditional technique, the flap is transplanted on 1 or 2 vascular pedicles, but modifications using microsurgery are also possible. For example, the TRAM flap “with pumping”, when vessels from the transplanted tissues and axillary vessels are additionally connected to improve blood circulation.
- Free abdominal flap (DIEP flap). It includes only skin and adipose tissue, and the vessels are connected to those supplying the chest (circumflex scapular, thoracodorsal, internal mammary vessels) using microsurgical methods. This operation is technically more difficult, but does not damage the abdominal muscle wall.
- There are methods for breast reconstruction using flaps taken from the buttocks or the iliac region, but in our country they are practically not used in reconstructive surgery.
The most common complication during breast reconstruction using one's own tissue is necrosis (death) of the transplanted flap. This occurs when the blood supply to the displaced tissues is not restored. Chemotherapy does not affect the survival rate of flaps, but radiation therapy worsens it, since it affects the vessels. In addition, the likelihood of necrosis is higher in conditions such as diabetes, obesity, diseases of the cardiovascular system, as well as in smoking patients.
Rehabilitation period
Depending on the type of operation and general condition, the woman stays in the medical center for three to six days. If there are no complications, the patient is discharged. The doctor gives a memo that indicates the basic rules of the rehabilitation period.
Recommendations:
- After the operation, you should not raise your arms, make sudden movements, or bend low. It is important to remain in bed until your doctor allows you to get up. You need to get out of bed carefully, do not overexert yourself,
- During the first few days you will experience painful sensations of varying intensity. As prescribed by the mammologist, the patient receives injections of analgesics, and later the oral form of drugs. To reduce the risk of inflammation, antibacterial compounds are prescribed,
- After removal of the drainage system, fluid accumulation may occur in the operated area. If there is a significant amount of secretion, the doctor extracts the contents using a puncture,
- In most cases, to completely suppress the tumor process, mastectomy is combined with chemotherapy or radiation. The choice of treatment method and timing is carried out by a mammologist-oncologist,
- in the absence of complications, a woman can lead a normal life after one and a half to two months, sexual contacts are allowed after the same period. It is important to limit lifting weights, do not sunbathe, do not visit the solarium, sauna and bathhouse,
- if there is no desire or financial opportunity for breast reconstruction, you can purchase an orthopedic bra, when worn, it is impossible to detect the absence of a mammary gland even in light clothing.
Find out about the first signs of papillary thyroid cancer, as well as about the treatment of cancer pathology.
This article explains what lactic acidosis is in diabetes mellitus and how to treat this dangerous complication.On the page https://fr-dc.ru/zabolevaniya/diabet/profilaktika.html, read useful recommendations from endocrinologists on preventing complications of diabetes in men and women.
Preventive mastectomy: personal experience
Anya, breast augmentation is a common thing. But you decided to reduce it. For what?
I had D size breasts since I was 18, and the sagging made them seem even larger. In addition, ptosis aggravated the load on the spine: my neck hurt, I slouched, and could not lie on my stomach. Therefore, I decided to have a reduction, which is considered the second most difficult operation after tumor removal.
How did it happen that you also had to have a mastectomy?
I have always been at risk: the whole family on my mother’s side suffered from cancer. My mother fought ovarian cancer, my grandmother fought breast cancer. When I told a plastic surgeon about my genetics in 2020, he suggested a mastectomy.
At first I was confused because I was consulting for another intervention. But then I took a BRCA1 test for the presence of major mutations in the genes, and the result showed an 85–90% chance of developing breast cancer and a 50% chance of developing ovarian cancer. And I agreed to have a mastectomy.
The recent loss of my mother gave me determination: I learned how unpredictable the disease can be.
Did you consult with other specialists?
Certainly. I went to the city of Ivanovo, to the hospital at Russian Railways - to a doctor whose mother had previously undergone minor plastic surgery. From there I was sent for a mammogram, ultrasound, and other tests. The surgeon also suggested consulting with a mammologist-oncologist at the Moscow Research Oncological Institute. P.A. Herzen. All the specialists were categorically against mastectomy, but could not offer anything concrete in return, other than periodic examinations.
Why were the doctors against it?
Very few surgeons around the world still perform such an operation. And for Russia this is a completely unexplored area.
Jumper, COS
But that didn't stop you.
No. I went for a second consultation in Ivanovo. There were three doctors there: the head of the surgical department, Sergei Nikolaevich Voronov, who advised me for the first time, mammologist-oncologist Maxim Valerievich Venediktov, and surgeon Natalya Sergeevna Voronova. Their opinions were divided. The men suggested doing a mastectomy, and Natalya Sergeevna advised stopping at a reduction. Her main argument was the impossibility of breastfeeding in the future. But they also explained to me that in large breasts, oddly enough, there is little milk and the baby has to be supplemented with formula. By the way, my mother also faced this problem.
Then they explained to me in detail the essence of the operation, told me about the consequences and two options with nipples. They were either removed and then made into imitation leather, or left. In the second case, there is a risk that the nipples will not take root. I thought about a month and a half. My boyfriend helped me decide. He advocated a mastectomy, believing that health and life were more important than breastfeeding. And at the end of February 2018, I had surgery.
Why did you decide not to wait until you give birth?
I never had clear plans to get married and give birth at such and such an age. Life is unpredictable. I wasn’t going to have children in the near future, which means I would have to wait for who knows how many years and the likelihood of getting sick would increase. After my mother’s death, I wanted to protect myself from this as much as possible. Therefore, I decided to have the operation while the body is young and it is easier to cope with such an intervention.
Tell me, what is the essence of preventive mastectomy?
It differs from the usual one in that not the entire breast is removed, but only the mammary glands, and implants are inserted in their place. Along with the mastectomy, I also had my breasts reduced. The operation lasted about four hours, and I spent a week in the hospital with constant IVs and injections. When I was discharged home, I was happy, but after a couple of days I realized that it was calmer in the hospital: the slightest change in my condition caused panic.
It hurt?
I didn’t feel any pain because I mostly slept all the time. But it turned out to be difficult to move: I had drainage tubes under my arms, from which fluid was periodically drained. Even after breast surgery, you cannot raise your arms for some time. Yes, they don’t rise, to be honest.
Did you expect it to be easier?
There was nothing to compare it with. Mastectomy is a complex operation and the recovery period is long. I felt completely healthy and strong after three to four months. At first you have no strength at all, neither physical nor moral, so it’s worth enlisting the support of your loved ones. I was lucky with this.
Who helped you?
My boyfriend, who at that time lived in Finland, spent all the days with me in the hospital and then helped me at home. Dad came back from a business trip. Every day my friends wrote to me, called me and visited me.
Dress, Patrizia Pepe; sneakers, Dior
What do your breasts look like now?
I'm size B-C. The stitches were T-shaped: around the nipple, down to the base and under the breast. The scars are still slightly visible, but can no longer be felt to the touch. I don’t feel the implants either, they have become a part of me.
You talked about your problem on social networks. How did people react?
I thought for a long time whether I should do this. I lay in the ward, waiting to be called into the operating room. The doctors took the necessary measurements, and I examined my painted neck and chest. Then I took a selfie and posted it in my story with the caption “here we go.” When I woke up after anesthesia, the phone was ringing.
I decided not to hide anything: when it was hard and scary, I honestly wrote about it. In response, I received only support. Then strangers began writing, wishing for a speedy recovery. It helped me a lot. But today I see that not everyone understands the meaning of my operation, so I will say again: this is not a solution to cosmetic problems or a fight against complexes, but a chance to prevent a terrible disaster.
Lifestyle
Helpful Tips:
- eat right, sharply limit the amount of fat and salt to reduce swelling. Get food with the optimal amount of proteins, vitamins, and carbohydrates. Vegetable fats, food is not spicy, almost unsalted, not very sweet, without preservatives. It is necessary to limit baking, white bread, and fast food. Pickles, marinades, mayonnaise, coffee, alcohol, fried foods are prohibited. You can't gain extra pounds
- psycho-emotional balance, support for loved ones, overcoming depression, reducing the frequency of stress, important elements of recovery, prevention of complications,
- with the permission of the mammologist, after complete healing of the scar, you can visit a sanatorium for a speedy recovery after surgery,
- Light physical activity is beneficial. Be sure to work out your arms and perform special exercises selected by a rehabilitation doctor. You should not overload the muscles, but lack of movement during the rehabilitation period leads to stagnation, swelling, and poor lymph movement. All exercises should be performed strictly with the permission of the mammologist, within the time frame specified by the doctor.
Possible complications
The use of modern methods of resection of affected mammary glands in combination with comprehensive rehabilitation reduces the likelihood of an inflammatory process and the spread of metastases. Strict adherence to the recommendations given by the mammologist reduces the strength of negative feelings after a mastectomy.
After surgery, some patients experience complications:
- the hand swells when the outflow of lymphatic fluid is disrupted,
- phantom pain in the surgical area,
- bleeding and poor wound healing,
- skin necrosis, contractures,
- decreased mobility of the shoulder joint,
- erysipelas of tissue with further degeneration into more severe forms: abscess, sepsis,
- depressive states, especially in the absence of desire or opportunity for breast surgery,
- curvature of the spine, causing pain in the cervical area and poor posture.
An important factor that reduces the risk of complications is cooperation with a qualified mammologist-oncologist and surgeon. Mastectomy is a difficult operation. Inaccuracies during the removal of the gland, the choice of an inappropriate method of surgical treatment without taking into account the individual characteristics of the patient can lead to dangerous complications. You need to find a high-level clinic and an experienced doctor. Most medical institutions that use the latest equipment and an effective set of measures during the rehabilitation period offer women reconstructive plastic surgery to eliminate cosmetic defects.
Lingerie Anita
Anita underwear has proven itself well and can be used immediately after surgery. It is very comfortable, especially during the postoperative period when there is swelling, pain and pressure in the chest. It provides:
- Comfortable sleep.
- Hiding scars and knots.
- Reducing the chances of breast compression.
Anita underwear provides a comfortable position for the breasts, while hiding damaged areas of the skin. If you do not take advantage of this offer, you may end up with the following consequences:
- Seams coming apart.
- Displacement of dentures.
- Bleeding and tears.
- Deformation of breast tissue.
The natural desire of women to look beautiful, even after surgery, is completely justified. However, it should be understood that failure to use special underwear can lead to undesirable consequences that simply disfigure the appearance. This will lead to even greater psychological trauma than simply removing one or two mammary glands.
Women have a choice:
- Use compression garments that support the dentures.
- Do not wear underwear, which will ensure long and uneven healing of seams and scars.
It is recommended to use the first option, since compression bras are made from natural elastane.
go to top