Causes of tear duct obstruction
Normally, after washing the eye, the tears of a healthy person flow to the inner corner. Through the lacrimal openings they pass into the lacrimal canal, flow into the lacrimal sac and exit into the nasal cavity. With dacryocystitis, this process is disrupted; the tear fluid, stagnating, loses its antibacterial properties, and infectious agents develop in it, causing inflammation.
In children, the reasons for the development of ophthalmological pathology are as follows::
- gelatin-like plug that did not resolve after birth;
- blockage of the tear duct;
- narrow lumen of the nasolacrimal passage.
In adults, dacryocystitis appears for the following reasons::
- swelling of the tissues of the nasolacrimal area due to nasal polyposis or sinusitis;
- traumatization of the lacrimal canal or the area next to it.
Mechanism of occurrence
The lacrimal sac is located between the inner corner of the eye and the bridge of the nose. The back part is in the bone notch, and the front part is under the skin. The lacrimal sac is connected to the nose by the nasolacrimal duct; through this duct, tear fluid exits into the nasal cavity. When for some reason this channel becomes clogged, the drainage of fluid from the lacrimal sac is disrupted.
As a result of a blocked tear duct, fluid from the eyes cannot drain normally through the nose. Gradually, the inflammatory process begins and bacteria actively multiply.
Dacryocystitis is a fairly rare phenomenon in adults; it is more common in women.
Classification and symptoms
Based on the nature of its course, dacryocystitis is divided into acute and chronic. Due to its appearance, obstruction of the lacrimal canal can be chlamydial, allergenic, traumatic, or viral. Clinical signs vary depending on the form of the disease.
Acute dacryocystitis has the following striking symptoms:
- swelling of the eyelid;
- fever;
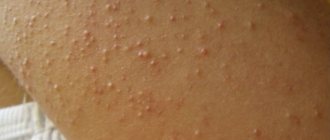
- compaction of the lacrimal sac, “fat lumps” near the eyes;
- hyperthermia of the skin near the lacrimal canal.
A constantly clogged tear duct leads to a rapid transition from acute to chronic dacryocystitis. This form is characterized by ongoing inflammation of the lacrimal sac. The resulting tumor softens, hyperthermia decreases, and an abscess forms, which can open on its own. Purulent exudate flows out of it, after which the inflammation subsides.
Treatment methods for swelling of the upper eyelid
Treatment of edema of the upper eyelid is directly related to its cause; depending on it, methods and treatment regimens will be determined.
- If it’s all about the inflammatory process, then they can prescribe antibacterial and anti-inflammatory drugs of systemic and local action, as well as physical procedures that enhance the effect of medications.
- In case of injury, if it occurred no more than a day ago, a cold compress is first applied to the eye. The open wound is treated with antiseptic and anti-inflammatory agents. To prevent the spread of infection, your doctor may prescribe antibacterial eye drops. Further measures depend on how extensive the damage is and whether other organs need to be treated.
- If swelling is caused by an allergy, you should definitely find out what exactly the irritating allergen is. The easiest way to do this is with allergy tests. After this, contact with the irritant is avoided as much as possible, and antihistamines are selected. In severe cases of an allergic reaction, hormone therapy is performed.
How to distinguish conjunctivitis from dacryocystitis?
Inflammation of the lacrimal sac is similar in external manifestations to many eye pathologies, including conjunctivitis. But when comparing the symptoms, certain differences can be identified. The following table shows the main differences.
| Sign. | Conjunctivitis. | Dacryocystitis. |
| Swelling of the eyelids. | Both eyelids swell predominantly and the swelling is insignificant. | There is swelling of the lower eyelid. If you press on the inflamed area, pus is released from the lacrimal openings. |
| Tearing. | Constant, but the tears are pure. The exception is bacterial conjunctivitis, in which there is purulent discharge in the tears. | Spontaneous and almost continuous (with pus). |
| Itching and burning. | They are characteristic symptoms. | Not observed. |
| Localization of pain. | The pain is localized throughout the eye or in its corner. | The source of pain is the lacrimal sac, which is located near the nose. |
| Temperature increase. | Absent. | Body temperature rises if inflammation affects blood vessels. |
| Spreading. | It gradually affects both eyes. | It is most often localized on one eye. |
What Causes Puffiness Above the Eyes
There can be many reasons for this condition. In general, they can be divided into three main groups:
- Loss of skin elasticity. This reason can be called one of the main ones. This is usually called aging of the body, since over the years the skin's ability to synthesize collagen decreases. The modern rhythm of life, when people sit for a long time in front of a monitor screen or gadgets and overstrain their eye muscles, only intensifies this process. By the way, some people have a genetic predisposition, although this cannot be solely blamed.
- Accumulation of fluid under the skin. This is exactly what many people habitually call edema. Watery bags usually indicate kidney problems. If such swelling occurs only once, then most likely the food consumed during the evening meal is to blame. Most likely, the person ate too much salty food at dinner. Sodium retains water in the body, and as a result, swelling appears in various parts of the body. They are more noticeable on the eyes, since even small (literally a millimeter) shifts towards increase in the tissue of the eyelids are very noticeable to others.
- Overgrown adipose tissue. Excess weight appears not only in the waist, hips and back. When overeating occurs, skin grows literally all over the body, including the eyelids. When losing weight, stretched skin cannot shrink on its own, and an excess of it appears. This looks like drooping eyelids or bags over the eyes.
- Allergy. Manifestations of allergies most often affect areas where there is mucous membrane (nasal cavity, eyes). This is how classic hay fever can manifest itself, which begins in the spring. But if only the eyelids swell, there is a possibility of an allergic reaction due to the cleansing and cosmetic products used by the person. Finally, food, as well as household items, including animal hair, cannot be excluded as an allergen.
- Infection in the eye. Conjunctivitis, stye, blepharitis and other inflammatory eye diseases can appear in different parts of the organ of vision. When pathogens are activated in the tissues of the upper eyelid, in response to inflammation, the body provides an increased influx of prostaglandins and lymphocytes. As a result, the tissue of the eyelid becomes dense, and the eyelid itself looks swollen.
- ENT diseases. Inflammatory processes in the nasopharynx negatively affect surrounding tissues. Metabolism in the latter worsens, and bags appear over the eyes.
A person’s lifestyle is of no small importance. In particular, your daily routine (or more specifically, your bedtime) can be critical. If you regularly violate the recommended norms (go to bed no later than 11 p.m.), even youth will not save a person’s beauty, and even in the morning he will look tired.
Some women also experience this condition at regular intervals. So, swollen eyelids may be a consequence of a hormonal surge - during (or on the eve of) menstruation or during menopause.
Diagnostics
The diagnosis of “dacryocystitis” is made after an external examination and anamnesis. Further examination includes:
- Vesta sample. A tampon is inserted into the nostril on the side where the inflamed lacrimal canal is located, and a collargol dye solution is instilled into the eye. If everything is normal with patency, then within a couple of minutes the tampon will be colored. If this does not happen after 10 minutes, the West test indicates that the tear duct is clogged.
- Probing. The study reveals damage to the lacrimal canaliculi.
- Bacterial culture of a smear from the nasolacrimal duct. Bacterial analysis is necessary to identify the infectious agent.
Treatment of dacryocystitis in adults
Therapy is carried out exclusively by an ophthalmologist. In adults, the question of whether dacryocystitis can go away on its own disappears due to the reasons that provoked the pathology. It will not happen .
Medicines
Treatment for acute and chronic forms differs. Therapy is carried out in a hospital. Self-treatment is unacceptable; home therapy can lead to worsening of the condition.
Acute dacryocystitis can be treated with antibiotics. Drugs are selected depending on the type of bacteria that causes dacryocystitis. Tobrex, Oftaquix, Levomycetin, Ciprofloxacin, Albucid are usually prescribed.
Instillation of antibacterial drops is performed. This is Gentamicin, Miramistin. Antimicrobial ointments are placed behind the eyelid. When an abscess forms, it is opened and drained, followed by washing the cavity with antiseptic solutions.
Sometimes medicinal leeches are used in treatment. It happens that hirudotherapy for dacryocystitis is the only remedy that helps pregnant women. After all, many drugs are prohibited for them. Depending on the course of the disease, a different number of sessions may be required. Usually 3-4 sessions are required.
Surgical intervention
Chronic dacryocystitis is eliminated surgically, during which doctors create a new passage between the nasal cavity and the lacrimal sac. This ensures normal drainage of fluid through the lacrimal canal. In the most severe cases, they resort to removing the lacrimal sac.
ethnoscience
Treatment with folk remedies should only be used as an addition to primary therapy. There are many remedies that will help fight dacryocystitis.
- Kalancho juice. It helps remove blockages from the nasolacrimal duct due to its local irritant effect. To prepare juice at home, fresh leaves of the plant are cut, washed, dried and put in the refrigerator for a couple of days. This achieves the maximum level of concentration of nutrients in the plant. Then squeeze out the juice using a blender or juicer and dilute it half with saline. The juice is dripped into the nose, 10 drops at a time.
When should you sound the alarm about swollen eyelids?
Bags under the eyes in the morning cause a bad mood for the whole day. Especially if an important event is to take place the day before. We look very tired, and no foundation can hide this defect.
Before you start dealing with swelling of the eyelids, you need to try to find out the root cause. Maybe the day before you were very stressed or overexcited? Or are you suffering from lack of sleep?
Nerves, worries - all this, sooner or later, leaves an imprint on our appearance. The skin suffers from a lack of oxygen, blood circulation is impaired, so it becomes thin, flabby, blood vessels become visible and bruises appear.
The skin of the eyelids is very thin and sensitive. It needs to be constantly moisturized and nourished with special gels or creams. The sooner you start caring for this area, the higher the likelihood that the first wrinkles will not come soon.
It is believed that a swollen eyelid after sleep is one of the most harmless types of this disease. Especially if this phenomenon is rare.
Reasons why eyelids swell
- The night before you cried a lot and were very stressed;
- Drank a lot of alcohol at the party;
- Drink a lot of water, tea or coffee at night;
- Poor nutrition, which causes exhaustion of the body;
- Bad habits;
- Genetic predisposition;
- You ate a lot of spicy or salty food;
- Allergy to cosmetics or night cream;
- Permanent makeup;
- Insect bite;
- Eye disease;
- Cold.
Scientists have found that women over 30 suffer from this disease most often. Excess fluid in the upper eyelid can also accumulate due to lack of fluid. You need to carefully analyze your diet and figure out the mistakes you are making.
If swelling of the upper eyelid is a rarity for you, and there are no changes in the eyeball and no unpleasant sensations (itching, pain, stinging), then in this case there is no need to sound the alarm.
What symptoms require immediate medical attention:
- Bruise or injury - accompanied by lacrimation, redness, and hematomas may appear. The eyes itch, there is a pain, it hurts to look at the light. The eyeball is red and blood vessels are visible.
In this case, urgent medical attention is required. Because a bruise can greatly affect your health! Take care of yourself. After all, even one accidental injury to the eye can lead to a lot of unpleasant consequences!
- Allergy - accompanied by sneezing, runny nose, rash and itching. An allergy can be to anything: pollen, dust, insects, cosmetics, food products. You should take an antihistamine and consult a doctor.
- Eye disease (styree, conjunctivitis, pathology of the lacrimal duct, meibomitis) - painful sensations, itching, discharge of pus. You should urgently contact an ophthalmologist who will prescribe you special drops and ointments.
- Diseases of internal organs - fluid retention leads to swelling. If swelling of the eyelid is a regular occurrence, which cannot be treated at home, then you should consult a specialist.
Diseases that lead to fluid retention in the body: hypertension, kidney dysfunction, diseases of the cardiovascular system, viral infections, disorders of the endocrine system.
- Pregnancy and menstruation - during pregnancy, a woman’s body is subject to hormonal surges. A lot of excess fluid accumulates in the body, a lot of stress is placed on the internal organs, and this can cause problems with the kidneys. If you notice that your eyelids are constantly swollen, then you should definitely go to the doctor!
During menstruation or PMS, there is a large production of the hormone estrogen, which has the ability to retain fluid in the body. If swelling of your eyes occurs only during this period, then you should not be afraid.
Dear readers, one of the main problems with swelling can be cosmetics. Moreover, both decorative and caring.
If you abuse products such as eyeliner, mascara, pencil, then you are at risk. Especially if the cosmetics are not of very high quality and, worse, have expired. Alas, such cases are not uncommon, so we remind you of this!
Always wash off your makeup before going to bed! If you notice allergic reactions, you should immediately stop using the product and switch to hypoallergenic cosmetics.
To remove make-up, it is best to use micellar water or hydrophilic oil. Forget about soap! It dries out delicate skin very much, which leads to its depletion and the appearance of early expression lines. Take care and love yourself, take proper care of your skin - it will thank you for it!
Features of therapy in children
A common cause of dacryocystitis in children is a membrane that should break at the first cry of the baby. If there is no rupture, the lacrimal canal remains sealed, and inflammation of the lacrimal sac develops.
Parents often wonder whether dacryocystitis can go away on its own in a child? Yes. Sometimes the film does not break immediately, but after a couple of weeks or even months, and the obstruction of the lacrimal canal resolves itself.
Massage of the tear duct
A pediatrician should teach parents how to effectively massage. There is nothing complicated about technology. You need to move your finger from top to bottom from the corner of the eye and the bridge of the nose (10 repetitions) with slight pressure. You need to finish the session with light vibration movements in the area of the lacrimal glands. It is necessary to carry out a special massage for 14-21 days.
The best drugs
Massage is combined with the following means:
- Albucid. Eye drops that effectively destroy the causative agent of dacryocystitis.
- Collargol. The drug is dripped 4 times a day until the condition improves.
- Signicef. An antibacterial drug belonging to the group of fluoroquinolones. For dacryocystitis, children over 9 years of age and adults are recommended to instill one drop every 2 hours for the first 3 days. Then 4 times a day for 5-14 days (to be agreed with the doctor).
- Furacilin. A well-known antimicrobial drug, the solution of which is recommended to wash the eyes with dacryocystitis to eliminate pus.
- Tobrex. An antibacterial drug that is used in courses, as addiction occurs and sensitivity to it is needed to be restored.
- Vitabact. Vitabact for dacryocystitis is used to wash the eyes. Judging by the reviews of experienced mothers, the drug is weak and gives a positive result in combination with Tobrex or Fucithalmic. Apply twice a day for a course of 10 days.
Homeopathy
Many traditional healers claim that they know how to cure dacryocystitis with homeopathic medicines.
For dacryocystitis, homeopaths recommend the following remedies:
- Argentum nitricum 30. 7 balls are dissolved in 1/3 glass of water. Give a teaspoon 7 times a day.
- Pulsatilla 6. The granule is dissolved in 1/3 glass of water and the solution is given a teaspoon to the child every 2 hours for 2 days.
- Silicea 6. This homeopathic remedy is alternated with Pulsatilla 6, conducting similar therapy every 2 hours until the condition improves.
- Argentum nitricum 12. One granule of the product is dissolved in a dessert spoon of water and given to the child once.
How to get rid of it: treatment methods
The preferred method to get rid of paint bags is cosmetic procedures .
It is worth noting! One of them is thermolifting. With this method, laser treatment of subcutaneous adipose tissue is performed with a laser without opening the outer layer of the epithelium.
This leads to a decrease in the volume of fat deposits and a tighter fit of the skin to the cheekbones, as a result of which the bags are visually reduced and the skin is smoothed.
A more common procedure for this problem is lymphatic drainage massage.
It can be done at home, but for greater effectiveness it is recommended to perform this procedure in a beauty salon.
The purpose of the massage is to enhance the outflow of lymphatic fluid that accumulates in the paint bags.
The procedure must be performed by a specialist because it is necessary to have an understanding of the lymph circulation pathways: stimulation of these particular areas is required.
Plastic surgery
The peculiarity of painting bags is that it is almost impossible to eliminate them using non-invasive methods, and even more so by masking them.
In case of severe deposits, only the intervention of a plastic surgeon will be effective..
Keep in mind! Modern medicine offers three options for such operations:
- Filling the nasozygomatic groove . It is used for small bags to level the relief by introducing fillers (synthetic implants), patient tissue or fat into the area of the painting bags. Obviously, in the absence of sagging skin and large swelling, such an intervention is not suitable.
- Check-lifting . This is a combination of blepharoplasty and skin tightening. The operation takes no more than half an hour under general anesthesia, and rehabilitation takes up to one month. But the result in most cases is positive, and in addition to eliminating paint bags, this method helps to rejuvenate the skin of the face.
- Liposuction. This is the most effective method in which fat and connective tissue are removed from under the skin, which contributes to the retention of excess fluid in this area and the formation of deposits. The method gives quick results, but this procedure must be repeated every few years, since with age, deposits in the cheekbone area will still form.
Each operation has contraindications that must first be identified.
The type of operation depends on the structural features of the patient’s skin and subcutaneous tissues and is determined individually in each specific case.
Injections
You should know! Injections are best used at the initial stage of the formation of paint bags.
For this purpose, the drug diprospan is most often used - a hormonal agent that destroys fat formations.
The drug has contraindications and is used with caution in elderly patients and people with thin skin.
The danger of diprospan also lies in the fact that if the dosage is violated, the drug begins to act not as a corrector, but promotes irreversible structural changes in the subcutaneous tissues.
The result is the opposite of the expected result.
An alternative type of injection is dermahil injections .
This is no longer a hormonal drug, but a composition containing synthetic peptides identical to natural substances produced by the epithelium.
This product helps smooth the skin and reduce bags by normalizing the functioning of natural regeneration mechanisms.
Gymnastics
Stay up to date! Gymnastics will not help get rid of paint bags, but it helps slow their progression and tones the skin.
To do this you need to do the following exercises :
- You need to close your eyes tightly and open them five or six times . With your eyes open, you need to fix your gaze for a few seconds on a pre-selected point or object located at a distance of 1-2 meters from the eyes.
- In a standing position, the gaze is shifted to one side as much as possible, fixed in this position for five seconds, and then in the same way moved all the way to the other side . Repeat 4-5 times.
- You need to stand by the window and blink quickly and as often as possible for ten seconds , without closing your eyes too much. After this, you need to close your eyes for a few seconds to rest and open them to look at a distant object outside the window, focusing your gaze on it.
- At the end of the set of exercises, you should rotate your eyes in different directions . Then you should move your gaze several times to the maximum position from side to side and from top to bottom (first in one direction, then in the other direction).
gymnastics three times a day or more often .
Important! The whole complex takes no more than five minutes, so if possible, you should do such exercises in any free time.
Folk remedies
As additional remedies for painting bags, you can use the following recipes:
- fresh cucumber along with its peel is grated on a fine grater and, dividing the resulting mass into two parts, each is wrapped in a separate piece of gauze in 2-3 layers. Once a day, such compresses are applied to problem areas for half an hour.
- Potatoes boiled “in their jackets” are peeled and mashed into puree, which is allowed to cool slightly. It should be hot enough, but not burn the skin. This puree is also wrapped in gauze and applied in the morning and before bed on the cheekbones for 20 minutes. After this procedure, you can wipe your face with ice cubes to enhance the tonic effect.
- From any natural fabric you need to sew two bags the size of a matchbox. A teaspoon of sea salt is placed in such bags , which can be purchased in pharmacies. Regular table salt is not suitable due to the low concentration of essential substances in it. The bags are used as compresses, but before applying them to the skin, they must be immersed in warm water for a few seconds. The procedure is performed once a day and no longer than 5 minutes.
- The easiest way is to apply beaten raw egg white to the area where the bags are formed . It is applied once a day for half an hour.
Note! These methods do not eliminate paint bags, but they can help slow their development or prevent their occurrence.
In such cases, traditional medicine can serve as an additional rather than primary method of treatment.
Prognosis, complications, prevention
Dacryocystitis is not often diagnosed in ophthalmological practice (only 5-7%). But despite its rarity, the disease poses many risks to the patient’s health. Dacryocystitis is not a fatal diagnosis. Its outcome and prognosis for the patient's future life are favorable.
Sometimes complications develop:
In this case, there is a risk of the patient becoming disabled. Preventive measures include timely examination and treatment of ENT organs, consulting a doctor if you receive cranial or eye injuries.
Video about the disease
Watch the episode of the “Live Healthy” program with Elena Malysheva, dedicated to the symptoms and treatment of dacryocystitis.
Author of the article: Bakhareva Elena Sergeevna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
If you find an error, please select a piece of text and press Ctrl+Enter.
The glands of the lacrimal system perform a number of functions that prevent the development of many diseases of the organs of vision. The secretion produced is needed to moisturize the mucous membranes of the nose and eyes, disinfect, nourish the cornea, and wash away microorganisms and foreign objects that have gotten under the eyelids. Violation of these functions (including those associated with inflammation of the lacrimal sac) is fraught with temporary or chronic vision loss, and therefore requires immediate consultation with an ophthalmologist and treatment.
Swelling of the eyelids above the eyes: how to treat with folk remedies
Swelling of the eyelids, also called “puffy eyes,” occurs for a variety of reasons. There are many ways to help eliminate this symptom at home. If the swelling does not disappear and is accompanied by other signs, you should consult a doctor to avoid the development of a serious eye disease. It is also necessary to strictly adhere to the dosage of drugs to prevent side effects.
- 1. Non-dangerous causes of eyelid swelling
- 2. Root causes
- 3. Folk remedies for treatment
Causes of inflammation of the lacrimal sac or dacryocystitis
The causes of dacryocystitis in children can be:
- “mumps” (acute mumps);
- scarlet fever;
- acute respiratory and infectious diseases;
- flu;
- pneumonia;
- tumors;
- neuroses.
- previous orbital and nasal fractures;
- eyeball injuries;
- damage to tear ducts;
- clogged eyes.
Contributing factors in adults are:
- tuberculosis;
- metabolic disorders;
- diabetes;
- weak immunity;
- working with chemicals.
Instructions for Visomitin eye drops are presented here.
Dacryocystitis can develop into a chronic form with syphilis, systematic pathologies of connective tissue, and Sjögren's Syndrome.
Symptoms for diseases of the orbit
Displacement of the eyeball relative to its normal location in the orbit: exophthalmos, enophthalmos, upward, downward displacement - occurs with injuries, inflammatory diseases, tumors, changes in blood vessels in the orbit, as well as endocrine ophthalmopathy.
Impaired mobility of the eyeball in certain directions is observed in the same conditions as previous disorders. Swelling of the eyelids, redness of the skin of the eyelids, exophthalmos are observed in inflammatory diseases of the orbit.
Decreased vision, even blindness, is possible with inflammatory and oncological diseases of the orbit, injuries and endocrine ophthalmopathy, occurs when the optic nerve is damaged.
Symptoms of the disease
There are chronic and acute forms of pathology. Chronic – divided into types, depending on the type of lacrimal gland disorders:
- aplasia (lacrimal gland is absent);
- hypoplasia (not fully formed);
- hypertrophy (increased in size).
The symptoms of the pathology are somewhat different. The clinical picture of the chronic type is manifested in:
- increased lacrimation;
- heat;
- discharge from the neoplasm of mucous and purulent exudate;
- swelling of the conjunctiva and lacrimal sac;
- painful sensations;
- narrowing of the palpebral fissure.
In the acute form it is expressed more clearly:
- the skin adjacent to the lacrimal sac turns sharply red;
- swelling appears, causing pain when touched;
- the palpebral fissures are completely or almost completely closed;
Signs of corneal inflammation and ways to eliminate it - viral keratitis of the eye.
In acute dacryocystitis, fever, general weakness, chills, eye pain, and fistula formation are possible.
Symptoms and treatment of viral conjunctivitis in adults are described in the article.
Treatment and possible consequences
The treatment regimen for adults and children is approximately the same, but pediatricians have their own methods of influencing the source of inflammation, taking into account the fact that the child himself will not sit quietly and may twitch violently due to pain. Such factors can significantly affect the state of the lacrimal drainage system and create conditions for the formation of fistulas and other complications. Therefore, therapy for inflammation of the lacrimal sac in adults is treated in its own ways, and in children - with slightly different methods.
In adults
It is worth mentioning that treatment of dacryocystitis should be carried out in a hospital setting, since there are risks to human life due to the development of sepsis. The patient is prescribed the following types of drugs:
- Anti-inflammatory hormonal and non-hormonal;
- Antibiotics;
- General strengthening.
Find out which antibiotics to use for conjunctivitis here.
Video shows treatment in adults:
Diagnostics
The diagnosis should be made by an ophthalmologist based on a visual examination, palpating the inflamed lacrimal sac and studying the patency of the lacrimal ducts using a canalicular test (Vesta). The latter procedure is based on inserting a tampon into the nose while simultaneously instilling a collargol solution into the eye.
With good patency, the pigment stains the tampon in 60-120 seconds, with difficult patency - within 5-10 minutes. A tampon that is not colored after 10 minutes indicates a blockage of the lacrimal ducts.
Children can undergo a passive nasolacrimal test.
But this article will help you recognize the symptoms of temporal arteritis and begin treatment.
In addition to probing the tear ducts, diagnostics include:
- living eye microscopy;
- fluorescein instillation test;
- bac sowing
Effective antimicrobial therapy - original and analogues of Vitabact eye drops.
How is diagnostics carried out?
If swelling of the upper eyelid has been bothering you for a long time, you should consult an ophthalmologist. Sometimes the reason for this phenomenon is obvious: after an insect bite, a pinpoint mark remains; traces of injury are also difficult to miss, especially since the patient usually knows whether something happened to him and can tell the doctor about it. In all other cases, a series of studies will be required to make an accurate diagnosis.
What diagnostic procedures should you prepare for:
- Visual inspection. The size of the swelling, skin color, density, presence or absence of rash, itching, burning, whether the eye opens or not is assessed.
- Instrumental examination. Biomicroscopy is a standard procedure - examination of the eyeball under a microscope for an inflammatory process. If necessary, the doctor will perform additional procedures: tonography, gonoscopy, pachymetry, etc.
- Laboratory blood tests. A detailed biochemical analysis will be required.
- Allergy tests.
- Ultrasound and electrocardiogram.
In order not to guess what exactly caused the allergy, you should undergo a simple test that immediately reveals a reaction to potential allergens
It is not necessary that all of them be appointed. But if the doctor has written out a referral for a consultation with a particular specialist or for additional tests, this cannot be ignored, even if it seems that such measures are not necessary. Many patients come to the doctor with a swollen eye and simply ask to be prescribed drops and tablets so that “everything goes away.” But sometimes such a symptom is a sign of a serious disease of an internal organ; eliminating it is pointless until the underlying disease is cured. And in order to establish exactly which one and select the correct, effective treatment, you will need to undergo an examination.
Treatment
The approach to eliminating the problem depends on the age characteristics of the patient.
In newborns
Treatment of dacryocystitis in newborns is carried out in stages:
- Massage for dacryocystitis in newborns (with reasonable effort, making 6-10 vertical movements after each feeding).
- Toilet the eyes by rinsing with furatsilin solution (1 tablet per 200 ml of hot water). The palpebral fissure is treated with a cotton swab soaked in the solution, moving from the temporal bone to the nomus. The final stage is the use of an antibiotic (levomycytin 0.25%).
A simple way to prevent any illness is vitamin eye drops.
In isolated cases, conservative treatment may not bring a positive result; then, under local anesthesia, a special probe is inserted into the lacrimal canal, and the paths are washed with an antiseptic solution. The procedure is safe, but requires preliminary preparation (general blood test, pediatrician’s report).
For instructions on Vitapos eye ointment, see the link.
In children
The acute form of inflammation in older children is treated in a hospital setting. Children are prescribed multivitamins and UHF therapy until symptoms of fluctuation are observed; later, the purulent inflammation is opened and drains are placed with a 10% sodium chloride solution. Over the next 3-7 days, the opening site is treated with antiseptics and lubricated with healing ointments. Massages are carried out at the same time.
For up to 10 days, use antimicrobial drugs (Gentamicin, Levomycetin, Tsipromed, etc.), antibacterial ointments, antibiotics:
- Oxacillin;
- Gentamicin.
- Cefotaxime;
- Cotrimoxazole.
- Urotropin;
- Solutions of hemodez, glucose 5%, ascorbic acid, calcium chloride 10%.
Positive trends from treatment should occur within 7-14 days, otherwise the lacrimal ducts are passively washed with a solution of furatsilin in a ratio of 1:5000.
If the healing process is not observed, manipulation is carried out using a Bowman probe under local anesthesia (for patients under 5 months) or under general anesthesia (for all others).
Operation
Children over 1 year of age can undergo balloon dacryocytoplasty. The operation involves inserting a thin conductor with a small liquid-filled balloon through the corner of the eye into the nasolacrimal canal. At the point where the channel is blocked, the balloon expands under pressure, clearing it. Infection is prevented by instilling eye drops and antibiotic medications prescribed by a doctor.
To prevent the formation of a purulent corneal ulcer during dacryocystitis, it is forbidden to touch the cornea. The taboo applies to any ophthalmological manipulations - ultrasound of the eye, wearing contact vision correction devices, tonometry, etc.
Find out how to treat inflammation of the cornea here.
Bags over the eyes
Causes of bags over the eyes
And of course, such a factor as lifestyle is of no small importance. An incorrect sleep schedule, sedentary work, lack of skin care around the eyes, constant nervous stress and poor nutrition lead to this problem. Liquid drunk in large quantities in the evening appears in bags the next morning. There may even be swelling of the face and lower extremities. However, under the eyes this manifestation disappears after a couple of hours.
Bags over the eyes can also appear as a consequence of other provoking factors:
Treatment
If no malfunctions are detected in the body, then it is necessary to make significant changes in lifestyle. To do this, some tips and recommendations will help:
Adequate sleep and moderate but constant physical activity, combined with proper nutrition, are the primary conditions for getting rid of the formation of bags over the eyes.
The use of traditional medicine provides good assistance in relieving swelling above the eyes. Among them, raw potatoes stand out, which are used both as compresses after squeezing out the juice, and by applying cut pieces to the upper eyelids.
Parsley juice . This is another effective remedy made from the greens of the plant. You can add a couple of drops of olive oil to this juice if desired.
Ice . Rubbing the eyelids in the morning with vitamin cubes helps the bags above the eyes quickly fall off. Ice can be made from chamomile infusion or parsley juice.
Fresh cucumber . Another means of quickly eliminating swelling. Cucumber can be used as compresses or by applying sliced circles to the eyes.
Tea brewing . Cotton mugs soaked in this product are applied to the upper eyelids. It is possible to use bags.
Prevention
Preventive measures include a systematic examination by an ophthalmologist and otolaryngologist, and maintaining eye hygiene. If the recommendations are followed, the likelihood of inflammation is minimal, and the treatment process proceeds without complications.
Inflammation of the lacrimal sac is a common painful process that occurs in people of any age. It requires immediate diagnosis and qualified treatment, otherwise it can have fatal consequences, including inflammation or brain abscess, purulent encephalitis and other similar complications.
Video
This video will tell you how to deal with inflammation of the lacrimal sac.
The presented material is for informational purposes only and cannot be considered as a basis for making an independent diagnosis. Before starting treatment, consultation with a specialist is required. In our other articles you can familiarize yourself with the causes of Fuchs syndrome.
Discharge from the eyes of a child with a cold: reasons why the eyes fester during ARVI and after sleep
Inflammation of the upper eyelid: causes and treatment in children and adults
Eye drops for newborns: which ones are best to use from birth
A newborn’s eye is festering - what to do, causes and treatment
Ardamakova Alesya Valerievna
Ophthalmologist, laser surgeon
Candidate of Medical Sciences
Eyelids are movable folds of skin that protect our eyes from dryness, dust, bright light and other negative factors of the surrounding world.
The top of the eyelids is covered with thin and delicate skin, penetrated by a large number of blood vessels.
Beneath the skin is muscle tissue that allows you to easily open and close your eyes.
At the back of the eyelid are the meibomian glands, which produce a liquid secretion to keep our eyes moist and improve the contact between the eyelids and the ocular surface.
The mucous membrane of the eye is lined by the conjunctiva with lacrimal glands, which contributes to additional hydration of the eyeball and protection against infections.
Inflammation of each of the organs that make up the eyelid causes the development of a number of characteristic diseases.
What is the skin above the eye called?
The key to good results when performing facial gymnastics and massages is accurate knowledge of facial anatomy.
The fight against aging for a woman usually begins with the skin around the eyes, since this is where the first age-related problems appear: the skin loses its freshness, swelling and fine wrinkles appear.
And no wonder: in the eye area the layer of epidermis is very thin - only half a millimeter. In addition, there are almost no sebaceous glands around the eyes, a “soft pad” of subcutaneous fat, and very little muscle to maintain its elasticity. Collagen fibers (the “reinforcement” of the skin) are arranged here in the form of a mesh, so the skin of the eyelids is easily stretchable. And due to the looseness of the subcutaneous tissue, it is also prone to swelling. In addition, she is constantly in motion: her eyes blink, squint, and “smile.” As a result, the skin around the eyes is particularly stressed. Therefore, let's start understanding the structure of the face from this area.
The eyelids and periorbital region are a single complex consisting of many anatomical structures that undergo changes during surgical manipulation
| 1 - Upper eyelid fold 2 - Upper eyelid groove 3 - Internal canthus 4 - Nasolacrimal groove 5 - Eyelid-cheek division | 6 - Lower eyelid fold 7 - Horizontal axis of the eye 8 - Lateral canthus 9 - Upper eyelid |
The skin of the eyelids is the thinnest on the body. The thickness of the eyelid skin is less than a millimeter.
Unlike other anatomical areas where fatty tissue lies under the skin, just under the skin of the eyelids lies the flat orbicularis oculi muscle, which is conventionally divided into three parts: internal, median and external. The internal part of the orbicularis oculi muscle is located above the cartilaginous plates of the upper and lower eyelids, the middle part is above the intraorbital fat, the external part is located above the bones of the orbit and is woven above into the muscles of the forehead, and below into the superficial musculofascial system of the face (SMAS). The orbicularis oculi muscle protects the eyeball, performs blinking, and functions as a “tear pump.”
| 1 - Frontalis muscle 2 - External part of the orbicularis oculi muscle 3 - Median part of the orbicularis oculi muscle 4 - Internal orbicularis oculi muscle 5 - Internal canthus 6 - Nasalis muscle, 7 - Levator labii muscle | 8 - Levator labii superioris muscle 9 - Depressor nasal septum muscle 10 - Zygomatic major muscle 11 - Zygomatic minor muscle 12 - Infraorbital nerve 13 - External canthus |
The musculoskeletal system of the eyelids performs a supporting function and is represented by thin strips of cartilage - tarsal plates, lateral canthal tendons and numerous additional ligaments. The superior tarsal plate is located on the lower edge of the upper eyelid under the orbicularis oculi muscle, and is usually 30 mm in length and 10 mm in width, it is firmly connected to the inner part of the orbicularis oculi muscle, the aponeurosis of the levator superioris palpebral muscle, Müller's muscle and the conjunctiva. The inferior tarsal plate is located on the upper edge of the lower eyelid, is usually 28 mm long and 4 mm wide, and is attached to the orbicularis muscle, capsulopalpebral fascia and conjunctiva. The lateral canthal tendons are located under the orbicularis oculi muscle and are firmly connected to it. They connect the tarsal plates to the bony edges of the orbit.
| 1 — Müller’s muscle 2 — Internal canthus 3 — Lacrimal sac 4 — Ligaments | 5 - Inferior tarsal muscle 6 - Lockwood's ligament 7 - External canthus |
Under the orbicularis muscle also lies the orbital septum - a thin but very strong membrane; one edge is woven into the periosteum of the bones surrounding the eyeball, and the other edge is woven into the skin of the eyelids. The orbital septum retains the intraorbital fat within the orbit.
| 1 - Orbital septum 2 - Internal canthus 3 - Intraorbital fat - central portion 4 - Ligaments | 5 - Intraorbital fat - external portion 6 - External canthus 7 - Lacrimal gland |
Under the orbital septum there is intraorbital fat, which acts as a shock absorber and surrounds the eyeball on all sides. Portions of the upper and lower intraorbital fat are divided into internal, central and external. Next to the upper outer portion is the lacrimal gland.
| 1 - Intraorbital fat - central portion 2 - Dividing septum 3 - Intraorbital fat - internal portion 4 - Internal canthus 5 - Intraorbital fat - internal portion | 6 - Intraorbital fat - central portion 7 - Ligaments 8 - Intraorbital fat - outer portion 9 - External canthus 10 - Intraorbital fat - outer portion 11 - Lacrimal gland |
The muscle that lifts the upper eyelid opens the eye and is located in the upper eyelid under the cushion of fat. This muscle is attached to the superior tarsal cartilage. The skin of the upper eyelid is usually attached to the levator palpebrae superioris muscle. At the site of attachment of the skin to this muscle, when the eye is open, a fold forms on the upper eyelid. This supraorbital fold varies greatly from person to person. In people from Asia, for example, it is weakly expressed or not at all; in Europeans, it is well expressed.
| 1 - Muller's muscle, 2 - Levator superioris muscle 3 - Superior rectus muscle 4 - Inferior rectus muscle 5 - Inferior oblique muscle 6 - Orbital bones 7 - Orbital margin 8 - SOOF - infraorbital fat 9 - Orbital ligament 10 - Orbital septum 11 - Intraorbital fat 12 - Capsulopalpebral fascia | 13 - Inferior pretarsal muscle 14 - Inferior tarsal plate 15 - Superior pretarsal muscle 16 - Superior tarsal plate 17 - Conjunctiva 18 - Ligaments 19 - Levator palpebrae superioris 20 - Orbital septum 21 - Intraorbital fat 22 - Eyebrow 23 - Eyebrow fat 24 - Bones of the eye socket |
Behind these structures is the eyeball itself, which is supplied and innervated through the posterior part of the orbit. The muscles that move the eye are attached at one end to the eyeball and lie on its surface, and at the other end they are attached to the bones of the orbit. The nerves that control the muscles are small branches of the facial nerve and enter the orbicularis oculi muscle on all sides from its outer edges.
The anatomical structures of the lower eyelid and midface are closely related, and changes in the anatomy of the midface affect the appearance of the lower eyelid. In addition to portions of periorbital fat, two additional layers of fatty tissue exist in the midface.
Why does swelling of the eyelid occur?
The skin's ability to stretch, loose structure and a large number of blood vessels lead to fluid quickly accumulating in the eye area.
There are various reasons for the appearance of swelling of the eyelids, but from the symptoms you can understand what triggered fluid retention in the body.
If the swelling of the eyelid is bilateral, combined with other edema of the body, and the skin on the eyelids is pale and cold to the touch, this indicates renal or heart failure, as well as severe anemia.
Swelling of the eyelid also occurs with head injuries and angioedema.
Many inflammatory eye diseases, such as the following, are also accompanied by swelling of the eyelids:
- stye, abscess, blepharitis, contact dermatitis and other inflammations of the eyelids;
- diseases of the paranasal sinuses;
- acute purulent, pseudo- and membranous conjunctivitis;
- phlegmon, acute dacryocystitis and other diseases of the lacrimal sac;
- ednophthalmitis, iridocyclitis and other pathologies of the eyeball.
Swelling of the eyelids (most often unilateral) is characterized by redness of the skin, pain on palpation and a local increase in temperature.
What symptoms to look out for
Puffiness above the eyes can vary. Based on external manifestations, it is possible to make a preliminary diagnosis with great certainty as to what triggered its occurrence. You should pay attention to the following symptoms:
- soreness or painlessness – if we are talking about ophthalmological diseases, most likely the eye hurts. Swelling caused by kidney problems, for example, usually does not cause physical discomfort;
- itching and burning - most often indicates an eye infection, allergy or reaction to an insect bite;
- when the eye swells, in the morning or evening, sometimes or constantly - it has already been said above that the causes of morning swelling are in most cases physiological, swelling in the evening indicates some kind of internal disorder;
- only one eye or both eyes swell - ophthalmic infections usually first affect one organ of vision, then the infection spreads to the other;
- does only the eyelid or other parts of the face swell, is there a rash, redness or blueness, lumps - all these additional symptoms are characteristic of various pathologies, allergies, inflammation, head trauma, etc.
It is important to understand that self-diagnosis is excluded in this case. Even if, after a thorough examination and assessment of the detected symptoms, you were able to presumably identify blepharitis, an allergy or another eye disease, the final diagnosis can only be made by a doctor after examination and questioning. He also prescribes the necessary treatment.
Causes of inflammation of the eyelids
Inflammation of the eyelids can be caused by the following reasons:
- pathological activity of mites living in the skin (a common phenomenon when the immune system is weakened);
- allergic reactions to certain types of medications, plant pollen, food;
- viral and microbial infections in the body;
- chemical, thermal and mechanical eye injuries;
- disruption of the cardiovascular and nervous systems;
- endocrine and hormonal disruptions.
Causes of swelling above the eyes
Swelling above the eyes will not go away and no cosmetologists will help until the cause of the swelling is identified and eliminated.
Edema in the human body is not considered normal #8212; therefore, it is a disruption of its normal functioning or a sign of illness. The reasons can be very different, from lack of sleep to inflammation of the frontal sinuses.
Swelling and hyperemia (redness) of the eyelids is a widespread pathology, and the reasons why the face or eyes swell can be divided into several groups:
- inflammatory and infectious processes;
- allergic reaction;
- non-inflammatory nature of edema;
- consequences of the injury;
- features of hereditary structure;
- Unhealthy Lifestyle.
Types of skin diseases around the eyes and eyelids
Among the huge number of diseases caused by inflammation of the eyelids, several of the most common groups can be distinguished:
- bacterial lesions of the skin of the eyelids (abscess of the eyelid, phlegmon);
- inflammatory diseases of the glands and edges of the eyelids (blepharitis, barley, chalazion, meibomitis, demodicosis);
- violations of the shape and position of the eyelids (entropion, eversion, ptosis, lagophthalmos);
- allergic diseases (eczema, dermatitis, angioedema);
- developmental abnormalities of the eyelids and tumors (coloboma, papilloma, lipoma, nevus).
Bacterial lesions of the skin of the eyelids
Abscess of the century
An abscess is inflammation and redness of the eyelid with the formation of a cavity filled with pus. Often an abscess appears after an infected eyelid wound.
Causes of eyelid abscess:
- ulcerative blepharitis;
- boils;
- barley;
- purulent processes in the paranasal sinuses and orbit of the eye.
Sometimes the abscess opens on its own, and the inflammation subsides. But in most cases, a non-healing fistula appears at the site of inflammation.
Treatment of an abscess is sanitation of the eyelids and opening of a purulent formation on the eyelids with the mandatory use of antibiotics and sulfonamides.
Phlegmon
Cellulitis is an extensive inflammation of the tissues of the eyelid that occurs against the background of untreated stye. It is characterized by fever, headache, severe swelling of the eyelid and redness of the skin.
Treated with antibacterial agents, antihistamines.
Inflammatory diseases of the glands and edges of the eyelids
Blepharitis
Blepharitis is an inflammation of the eyelids, which causes redness, burning, itching and pain on the skin.
The following types of blepharitis are distinguished: allergic, meibomian, demodectic, infectious, scaly. Read more about blepharitis here.
Barley
Barley is an acute, infectious inflammation of the eyelids, resulting from pathogens entering the eyelash hair follicle or the sebaceous gland of the eyelid. Visually, stye looks like a small nodule on the eyelid.
You can read about how to properly treat stye on this page.
Meibomyitis and chalazion
Meibomyitis and chalazion are diseases associated with the appearance of a pathological process in the meibomian glands.
Meibomia appears when the duct of the sebaceous gland of the eyelid is clogged. Characterized by an acute course of the disease.
Chalazion is a chronic form of meibomitis. If a chalazion is left untreated for a long time, it turns into an eyelid cyst. Sometimes, for diagnostic purposes, it is necessary to puncture the eyelid cyst to identify the nature of the neoplasm.
Causes of bags under the eyes
Bags are accumulated fluid under weakened eye skin. Determining the reason why they formed will help you understand how to not only prevent their formation, but also say goodbye forever.
There may be several reasons, and the most common of them are fatigue and regular lack of sleep.
This type of problem may also indicate that its owner has serious health problems. In this case, it is better to undergo a medical examination as soon as possible.
Weight problems can also contribute to the formation of bags. After all, if a lot of fat accumulates, the thin skin near the eyes is simply not able to support such weight, and therefore it bends and turns into a pouch.
Heredity also plays a role in the formation of unfortunate formations under the eyes. An anatomical feature or an unkind joke of nature may well be the cause of the appearance of such an unaesthetic disease.
In this case, traditional medicine will be powerless, and to solve the problem it is necessary to turn to plastic surgery and perform the blepharoplasty procedure.
If you do not have problems with genetics, and the reason lies in the factors described above, removing bags under the eyes will not be difficult.
Regular exercise, massage and all sorts of ways to use folk panacea will do their job and delight you with the result!
One of the few most effective massage effects is, at first glance, banal tapping with fingertips on the eyelids. The main thing is not to forget about the tenderness of the skin around the eyes.
Accordingly, massage movements must be done carefully. Do not damage the skin, beware of stretch marks. First, thoroughly clean your eyelids of makeup and dirt.
Apply moisturizer to the eye skin and gently tap with your fingers. This should be done as if driving the cream from the outer corners to the inner areas of the eyes. By performing this massage daily, you will notice how the condition of your eyelids improves.
Exercises to get rid of under-eye bags are good. First of all, those that will help preserve your vision:
1) Hold your head straight and raise your eyes up and then down. Look to the left and then to the other side without turning your head. Repeat the exercises ten times, then close your eyes and relax as much as possible.
2) Close your eyes as tightly as possible, and then open your eyes sharply and as wide as possible. Then close your eyes again and open them as much as possible again. Repeat ten times in a row, then rest.
3) Blink your eyes quickly for ten to fifteen seconds, close them and allow them to rest. Perform the exercise in two or three approaches.
In addition to exercises and massage, traditional medicine comes to the rescue, which is sometimes not inferior even to newfangled salon procedures. Therefore, recipes from “grandmother’s chest” should be considered and adopted by everyone.
Treatment of skin diseases around the eyelids
If suspicious inflammation in the eyelid area, redness, or pain appears, you should consult an ophthalmologist. After the examination, the doctor will make an accurate diagnosis and explain what to do for eyelid swelling and other symptoms, prescribe adequate treatment, and recommend preventive measures. This can be a massage of the eyelids with rinsing of the lacrimal ducts, opening of formations on the eyelid, the use of ointments and medications.
Ophthalmologists at the MedicCity clinic will quickly find the cause of your eye disease.
Come to us, we will take care of your vision!
If you have any questions, call us at:
First, the reasons
The appearance of swelling of the lower eyelid and sub-eye area, called bags, is preceded by several factors. First of all, this is an unhealthy lifestyle and all its components. Such as:
- unbalanced, unhealthy, insufficient or excessive nutrition (overeating);
- catastrophic and regular lack of sleep;
- sitting for days at a monitor or screen;
- lack of physical activity and fresh air;
- the presence of excess salt or liquid in the diet.
In a good way, before rushing to treat the bags, this “five” should be excluded from life. This will be useful not only for getting rid of bags. And at the same time, bad habits, like two glasses of wine before bed and a pack of cigarettes a day. But we won’t get carried away with science fiction. Let's try to get rid of at least one factor. Are the bags missing? Let's neutralize the next one. Are you present? We'll get through one more. To no avail? Let's say goodbye to one more thing... What if suddenly (lo and behold!) all the negativity and harm from life went away, but the bags remained?
Then it could be hereditary.
Or part of the natural aging process. The fat layer “melts” and “flows” down, the skin “does not hold” it, sags, and bags form.
We have already mentioned chronic diseases. Another cause of edema may be an allergic exacerbation.
Too many reasons? But there are many ways to get rid of it. Let's start with homework.