What is psoriasis?
Psoriasis is a fairly widespread chronic skin disease, characterized by the presence of a monomorphic rash in the form of pink-red nodules with a loose silvery-white scaly surface. The disease lasts for years, alternating periods of relapses and remissions are observed.
Typically, this disease causes the appearance of dry, red spots raised above the skin surface, but some people with psoriasis do not have visible skin lesions. These spots, called psoriatic plaques, in most cases first form on places that are subject to pressure and friction - the buttocks, the surface of the knees and elbows.
However, they can also be located and occur on other areas of the skin, including the palmar surface of the hands, the scalp, the external genital organs, and the plantar surface of the feet. Psoriasis is a chronic disease, usually characterized by an undulating course. The patient may have both periods of improvement and remission (caused by therapeutic methods or unexpected), and periods of exacerbations or relapses (most often provoked by unfavorable external factors - stress, alcohol consumption).
The severity of the disease in different patients, or even in one patient during periods of exacerbation and remission, can vary widely - from local small damage to complete coverage of the body with psoriatic plaques. Often, over time, progression of the disease is observed (especially in the absence of treatment), an increase in the affected area with the involvement of new areas of the skin, exacerbations become more frequent and more severe. Some patients may experience a continuous course of the disease without unexpected remissions.
The fingernails or toenails are also often affected. Nail lesions can occur in the absence of skin lesions and be isolated.
initial stage
Initial stage
The disease has an individual nature of manifestations, due to a genetic predisposition to skin regeneration, the strength of the immune response and the degree of development of the pathology. However, there are certain stages of psoriasis that are common to all patients:
- initial stage;
- stage of progress;
- stationary stage;
- regressive stage.
These stages develop cyclically and are observed in all patients susceptible to psoriasis. The disease occurs at any age, but the nature of its occurrence is not fully understood; most often, experts identify a hereditary factor as the source of the development of the pathology. Immune changes in the body’s protective activity lead to disruption of the life cycle of cells; they begin to divide unnaturally quickly, without having time to die off naturally. Thus, psoriatic plaques are formed and epidermal scales accumulate.
The first stage of psoriasis is characterized by the initial manifestations of signs of the disease: small inflammations appear in the form of blisters. Small plaques are localized on different parts of the body:
- skin under the scalp;
- palms and feet;
- armpits;
- elbow and knee bends;
- groin area.
Psoriasis develops quite quickly in the initial stage, affecting new areas of the skin every day. However, if the disease has not previously parasitized the human body, psoriasis at an early stage remains in one state for a long time, and the resulting papules in this case are called sentinel papules. Psoriasis at the initial stage has certain symptoms:
- rashes appear in places where the skin is most sensitive;
- small inflammatory lesions have a pink or reddish tint;
- the infection causes severe itching;
- the affected areas are covered with small scales of keratinized epidermis.
Psoriasis can be confused at an early stage with allergic dermatitis, since visually the pathology data are similar. Therefore, only a dermatologist can diagnose the disease and prescribe competent treatment, taking into account endocrine concomitant diseases and the general condition of the patient. Since psoriasis cannot be cured, the doctor prescribes individual therapy that promotes long-term regression.
The initial stage of psoriasis involves treatment with drugs of the glucocorticoid group. Typically these are creams and ointments that provide comprehensive symptom relief:
- relieving skin itching;
- suppression of the inflammatory process;
- reduction of peeling and the appearance of new affected areas;
- protection of the skin from secondary infections;
- regeneration of the epidermis.
Complex treatment may include the following stages:
- Popular non-hormonal drugs include Prednisolone, Dithranol, Akriderm, Cortisone. The first stages of the appearance of psoriasis with this treatment reduce their activity, although the use of the drugs can be very long. When used correctly medically, these drugs relieve inflammation, reduce itching and swelling, and also have an immunosuppressive effect.
- In addition, the initial stages of psoriasis are treated with ointments with zinc pyrithione, since the risk of side effects is low, and the therapeutic effect is quite significant (for example, Zinocap): moisturizing, softening, cell regeneration and anti-inflammatory effect.
- A special therapeutic diet is used that excludes allergenic foods, fried, fatty and spicy foods.
The initial stages of the formation of psoriasis on the body are manifested by the smallest area of damage, while the severe degree of damage spreads throughout the entire skin, affecting and deforming even the joints. At the initial stage of the disease, the patient is prescribed spa treatment, which significantly relieves the manifestations of psoriasis.
Stages of psoriasis
One of the most important elements in the clinical picture and course of psoriasis is its division into stages. If for acute diseases this is less important, then in the case of chronic pathology, a clear identification of stages is extremely necessary. After all, in this way it is very easy to assess the course of the disease, determine its sensitivity to a specific treatment method and choose further tactics for managing patients with psoriasis.
The following stages of psoriatic skin lesions are distinguished:
- Progressive stage of psoriasis;
- Stationary stage of psoriasis;
- Regressive stage of psoriasis;
Progressive stage of psoriasisShe says that the disease is beginning its next exacerbation. After all, psoriasis is characterized by wave-like development. Clinically, the progression of the process can be recognized based on the following signs:
|
Stationary stage of psoriasisIt is an indicator of a reduction in inflammatory skin changes. These data indicate the effectiveness of the treatment and the need to change it to less aggressive methods. Clinical features of the stationary phase of psoriasis are:
|
Regressive stage of psoriasisThis is perhaps the most pleasant moment in the treatment of psoriasis, both for the patients themselves and for the attending physicians. She says that the exacerbation of the disease has been practically defeated and the main task for the near future will be to prevent further exacerbations. Signs of the regressing stage of psoriasis are:
The stage of psoriasis is based on the activity of the inflammatory process. The pattern of clinical manifestations is that the more pronounced the redness of the skin, the more active it is. |
Why determine the stage and severity of psoriasis?
The doctor prescribes appropriate therapy depending on the severity and stage of the disease. For example, a patient with moderate to severe psoriasis may not need local therapy alone. Therefore, the doctor can prescribe systemic treatment: non-biological or genetically engineered biological drugs (GEBP).
Psoriasis is a chronic inflammatory non-infectious skin disease associated with excessively rapid division of cells in the outer layer of the skin - the epidermis. Psoriasis is accompanied by the development of inflammation in the skin, which is caused by immune disorders. As a result, accelerated growth and division of epidermal cells, multiple biochemical, immunological and vascular changes are observed. All these processes occur against the background of carriage of certain genes predisposing to psoriasis. Therefore, this skin disease is a genetically determined disease.
The development of debut and/or exacerbation of psoriasis occurs under the influence of provoking factors, including:
- errors in diet;
- alcohol abuse;
- taking certain medications;
- damage to the integrity of the skin (the so-called Koebner phenomenon);
- psycho-emotional stress;
- suffering from acute or exacerbation of chronic diseases;
- injuries, surgeries, etc.
Psoriasis has a rather complex nature, and the clinical manifestations of the disease develop under the influence of a number of external factors in people with a genetic predisposition.
Symptoms of psoriasis
Classic symptoms of psoriasis include raised patches of skin that are red and covered with a silvery-colored flaky crust. They usually form on the elbows and knees. There are several types of psoriasis. Their symptoms can come in different combinations and vary in intensity. The most common symptoms of psoriasis are:
- Bright red psoriatic plaques, often covered with flaky crusts of a silvery hue. They can occur anywhere, but, as a rule, they are localized in the elbows, feet, lower back, knees, and hands. Approximately 90% of people with psoriasis have a similar symptom.
- Small bleeding areas located in places where the flaky skin completely peels off or breaks off.
- Nail problems are a very common symptom, especially in severe forms of the disease. Small dimples appear in the nails, the end of the nail separates from the nail bed, and the toenails or in some cases the fingernails become yellowish discolored.
- Itching, especially during spontaneous outbreaks of the disease or when the plaques are localized, for example, under the buttocks or breasts.
Symptoms of psoriasis may also include:
- Similar plaques located in the same places on both sides of the body.
- Outbreaks in which a large number of droplet-like plaques appear.
- Joint pain, sensitivity, swelling.
The course of this disease can be divided into several stages. The first stage begins with an exacerbation, when there is a constant increase in the number of fresh rashes. The second stage is the stationary stage, in which the pattern of rashes remains unchanged, they do not become smaller or larger.
Regression is the third stage, characterized by the absence of rashes. A person affected by psoriasis feels suffering not only from external manifestations - red papules and crumbling scales. Patients are forced to experience unpleasant sensations from itching, which appears periodically.
The general condition of the body with psoriasis remains unchanged, the disease does not affect the usual way of life, and does not require being in any specific conditions. But still, this is a serious, aesthetically unattractive skin disease, and if the process of its development is not controlled, it will entail a lot of inconvenience and restrictions, such as, for example, the inability to wear short sleeves or sunbathe on the beach.
There is also a danger of increased itching; when scratching, difficult-to-heal wounds are formed. If left unattended, psoriasis can spread to the joints, leading to psoriatic arthritis, in which the joints of the bones become painful or swollen.
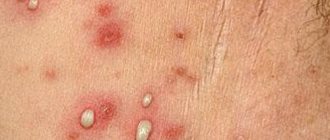
Progressive stage
Progressive stage
Progressive psoriasis is characterized by the formation of many sores of various shapes and sizes. The causes of exacerbation of the disease may be the following factors:
- severe stress and emotional overstrain;
- infectious diseases;
- exacerbation in the cold season is a common winter type, in which case the progressive stage is triggered by climate change, which gives rise to psoriasis;
- severe damage/trauma to the skin;
- long-term use of antibiotics;
- food allergens contained in products (honey, nuts, egg and chicken whites, milk protein, berries, citrus fruits);
- alcoholism.
The symptoms in which widespread psoriasis develops have distinct features:
- The skin becomes covered with spots that connect with each other and occupy a large affected area. This accumulation of plaques causes severe itching and flaking.
- Gradually, layers of dead epithelial particles accumulate, and plaques begin to rise above the surface of the skin. Severe swelling develops, psoriasis acquires a grayish tint, and the progressive stage reaches its peak.
- The swelling becomes severe, causing unpleasant pain.
- Whenever the affected areas are touched or damaged, angiogenesis, or the formation of small, thin capillaries capable of bleeding, is observed.
- The Koebner phenomenon develops, in which rashes become profuse when the skin reacts to various microdamages: scratches, cuts. The progressive stage differs from others precisely in this reaction of the body.
The duration of pathological manifestations takes from two weeks to several months, this may depend on how long and how the treatment lasts.
Treatment of the progressive stage of psoriasis is based on complex therapy, including the simultaneous use of medications, physiotherapeutic procedures and diet. Among the methods of complex treatment of psoriasis, the following can be distinguished:
- The progressive stage is expressed by the active growth of psoriasis plaques; with the help of a targeted ultraviolet laser, the growth of the affected cells is reduced, and the disease no longer progresses. Photoactive substances are used together with drugs to provide an anti-inflammatory effect.
- Preparations containing retinol, belonging to the vitamin group, can suppress psoriasis in cases where the progressive stage is not yet clearly expressed (Etretinate, Acitretin). These agents prevent cell division and the development of a bacterial background, which leads to the restoration of the epidermal layer.
- Treatment with steroids in the progressive stage of psoriasis is prescribed only for medical reasons, because they can cause adverse reactions in the body. However, such drugs have an anti-inflammatory, vasoconstrictor effect, and are also antiallergic drugs and immunosuppressants (Betamethasone, Dexamethasone, Metypred, Medrol).
- Widespread psoriasis must be suppressed with sedatives, since the progressive stage causes severe itching and nervous tension.
- For inpatient treatment of severe progression, the patient is prescribed intravenous administration of a 30% sodium thiosulfate solution and hemodesis three times a week. In addition, daily intramuscular use of potassium gluconate solution is indicated. Sorbents for removing toxins and emollient ointments are also prescribed.
- Vishnevsky ointment and salicylic ointment can be used as auxiliary anti-inflammatory agents.
- It is necessary to limit the body from any allergens, which means that with psoriasis, chemicals of any kind, cosmetics, and contact with animals are excluded.
When using folk remedies and tinctures containing alcohol, psoriasis will only progress, and the skin will be dry, and the formation of crusts will confirm the progressive status of the disease. Tar soap and tar-based products are also contraindicated, as it can irritate inflamed skin. Instead, it is better to use compresses with sea mud. The progressive stage involves a very strict diet that excludes different food groups. Physiotherapeutic procedures are prohibited at this stage; it is necessary to wait until the inflammation subsides.
Causes of psoriasis
Psoriasis cannot be contracted through a handshake or through household and personal hygiene items. The disease appears between the ages of 18 and 25 years. It appears as large spots on the skin, located anywhere on the human body.
Stress is considered a fairly common cause of exacerbation, development or occurrence of the disease. Psoriasis can be triggered by varying degrees of emotional shock. To date, the reliable causes of psoriasis are not known.
Possible causes of psoriasis include disruption of the endocrine system, changes in immunity, severe shocks and hereditary predisposition, although this area has not been fully studied.
The only thing that can be identified for sure is the mechanism of the appearance of psoriatic rash. It is based on an immune imbalance. It is a disruption in the normal functioning of the immune system, in which the body's cells and antibodies begin to show aggression towards its own tissues. And since the skin is one of the mirror images of the general state of health, it is most often affected by any autoimmune reactions.
On the subject: the best foods that boost immunity
The following factors can lead to such a strong immune imbalance in the body:
- Genetic predisposition. The risk of developing psoriasis is much higher among immediate relatives, especially first-degree relatives;
- Severe stress or constant mental stress;
- Diseases of the endocrine system;
- Metabolic disorders, vitamins and microelements. In this regard, it is especially worth dwelling on silicon deficiency in the body;
- Intestinal parasites;
- Viral infections.
There is no need to dwell separately on all the listed reasons, since there is more than enough information of this kind in various sources. It is worth pointing out the new elements that scientists have established regarding the etiology of psoriasis.
Parasitic diseases
Numerous studies have revealed a direct connection between infection with parasites that live and multiply in the intestines and the incidence of psoriasis. It turned out that the number of carriers of parasitic infections is much higher among patients with psoriasis than on average among healthy people.
A special role among these pathogens belongs to roundworms, lamblia, whipworms, bovine and pork tapeworms. Their role in the development of the problem is explained by the fact that when they exist in the intestines for a long time, toxic products of their vital activity are constantly released into the blood. They have high allergenic abilities, which lead to immune imbalance. The result is psoriasis.
Silicon deficiency in the body
Another important point among the causes of this disease can be considered a deficiency of silicon in the body. This pattern was established on the basis of a spectral analysis of the blood of patients with psoriasis.
It turned out that this microelement plays a very important role in the body, in particular in the structure of the skin, blood vessels and connective tissue. Its deficiency can be caused by poor soil and impaired absorption from the intestines. Again, the main role in this case belongs to intestinal parasites, the growth of which consumes almost all the silicon that comes from the external environment.
Read more: Flint water - a remedy for 100 diseases
Regressive stage
The last stage of psoriasis is called regressive. This period is characterized by attenuation of symptoms. Peeling practically disappears, plaques become flat. Scars are not formed; pigmentation of the skin in the affected areas may occur. Treatment at this stage is usually not required.
It is worth noting that the stages of psoriasis are distinguished conditionally. Even a specialist cannot always determine accurately, so careful monitoring of the patient is required. Treatment should begin immediately after diagnosis to avoid a more severe development of the disease.
Hemoscanning as a diagnostic method
A new direction in the diagnosis of psoriasis, which is widely advertised almost everywhere, is hemoscanning of blood. Different sources provide the most contradictory data. The primary goal of this article is to critically analyze all possible options and draw constructive conclusions from the abundance of information. About everything and in order.
The essence of the hemoscanning method is a visual assessment of blood. This procedure requires a special electron microscope with a high degree of magnification, and only one fresh drop of blood from the person being examined. In this case, the assessment is made instantly, since the blood is placed under a microscope, and the resulting image is displayed on the monitor screen. In this way, you can examine the structure and relationship of the formed elements and plasma, and identify signs of changes characteristic of psoriasis. The patient can be present during this study, listening to the comments of the diagnostician. The method refers to diagnostic techniques of alternative medicine.
Based on the data described above, we can conclude that the method is simply ideal for diagnosing almost all diseases. After all, without unnecessary numerous studies, you can get detailed information about your health in a short time. This is the point that is alarming regarding its reliability. This is used by many scammers who, thanks to it, promote their drugs and dietary supplements. But we should not forget that the method actually has a fairly good scientific basis and really helps to roughly determine the supposed qualitative changes in the blood that are characteristic of many diseases. Psoriasis is included in their list.
Hemoscanning is a fairly good method for monitoring treatment and controlling the activity of the inflammatory process in psoriasis. It is unacceptable to use it as the only method. It must be complemented by various diagnostic methods of traditional medicine.
Classic diagnosis of psoriasis
Psoriasis is diagnosed by a dermatologist or therapist based on external signs. The disease is easily recognized by the characteristic location of the lesions on the body. Usually, a clinical examination is sufficient; the diagnosis is always unmistakable, since a patient with psoriasis has skin changes that are typical only for psoriasis. If the picture of the disease is unclear, especially at an early age, then additional studies may be required, namely a skin biopsy.
In this case, a small piece of skin is taken and the pathologist examines the tissue sample and gives a conclusion. There is no blood test for psoriasis, because the blood retains its physical properties. The exception is severe psoriasis, spreading over the entire surface of the body, contributing to dehydration and disruption of the water-salt balance of the blood.
If a patient has pain or swelling in their joints, they may be tested for psoriatic arthritis. Any specialist in diseases of the skeletal system, after an X-ray and a blood test, will prescribe the correct treatment, preferably this should be a timely measure
Predisposing factors and onset
Psoriasis is one of the most common chronic skin pathologies in the world, and the problem of treatment still remains relevant. According to statistics, as of 2020, 130 ml of cases were registered in the world: every twenty-fourth inhabitant of the planet suffers from the disease. Typically, the onset of pathology occurs at ages from 16 to 20 and from 40 to 60 years. In 65% of patients, it is observed in a mild form, and the surface of the skin is slightly affected by plaques (up to 3%). Moderate psoriasis affects 25% (up to 10% of the skin area) and severe psoriasis, in which more than 10% of the surface is affected, affects 8%.
The exact cause of the disease has not yet been studied. It is assumed that the appearance of psoriatic plaques can be triggered by a parasitic infection, an allergic predisposition, hormonal imbalance, metabolic disorders and heredity.
The tendency to develop psoriasis in childhood, if one of the parents is sick, is 25%. When both – the probability increases to 50%. According to statistics, out of 100 children in the world, 4 of them suffer from psoriasis, and cases of the disease in boys are 25% less common than in girls.
The list of unfavorable factors also includes previous infectious diseases, neuropsychic injuries, and the negative effects of low temperatures.
As a result of the interaction of several external and internal causes, a disturbance in the blood circulation of the papillary layer of the dermis occurs, from which the reproduction of young and insufficiently mature epidermal cells occurs so quickly that they, without having time to fully mature, accumulate on the surface in silvery-white scales with a plaque-like or drop-shaped shape.
The disease progresses so much that over time they merge and turn into large spots.
Psoriasis lasts a lifetime and cases of self-healing are rare. Periods of remission alternate with exacerbation, which is more often observed in autumn-winter. But there are cases of an indeterminate (all-season) and photosensitive (summer) type.
Is psoriasis transmitted?
The question of the possibility of transmission of psoriasis from sick people to healthy people does not lose its relevance. This is due to the fact that patients with common forms of psoriasis look very noticeable against the background of the general mass. Not everyone understands that this disease is strictly individual and should not cause concern for others. This raises a lot of different types of questions:
- Is psoriasis contagious through contact? Numerous studies have found that psoriasis is not transmitted through direct contact under any circumstances.
- Is psoriasis transmitted sexually? Sexual relations with patients with psoriasis are absolutely safe, since this disease is a purely individual feature of the diseased organism.
- Is psoriasis transmitted to children during pregnancy? Pregnancy and childbirth are not directly related to the transmission of the disease from mother to child.
- Is psoriasis inherited? Genetic predisposition is one of the reasons for the development of psoriasis. The higher the risk, the closer your relatives have psoriasis.
Stationary stage
Stationary stage
The stationary stage of psoriasis development does not have clear time boundaries, but the patient’s condition is significantly stabilized. Symptoms of the disease at this stage have the following signs:
- the chaotic spread of plaques throughout the body stops;
- the feeling of itching remains, but it is significantly less than at the progression stage;
- inflamed pink areas are not visually observed, since they are completely covered with a dense layer of scales;
- the affected areas occupy a large area, the skin becomes coarser and becomes grayish in color.
This form of psoriasis is also called stationary due to the absence of symptoms of the Koebner phenomenon when the skin is damaged.
At this stage of psoriasis, treatment should be selected correctly, otherwise regression towards the previous stage can be observed. Medical indications for the presence of skin roughening include treatment of psoriasis according to a general therapy regimen. The stationary stage involves a therapeutic effect from the use of creams and ointments:
- glucocorticoid/hormonal ointments;
- ointments with zinc oxide, boric acid or tar;
- lotions with high retinol content;
- medicines based on tar, oil (ointments and shampoos)
At this stage, applications and baths with infusions of medicinal herbs also help relieve the symptoms of the disease: chamomile, St. John's wort, oak bark, string. Some traditional medicine recipes suggest honey compresses on the affected areas, but before using such therapy it is better to consult a doctor.
A complex of physiotherapeutic measures effectively suppresses psoriasis; the stationary stage of the disease involves the following treatment procedures:
- phototherapy (quartz treatment);
- laser/light therapy;
- cryotherapy achieves regression of the hospital, psoriasis weakens its development when working with low temperatures.
In addition, therapy methods such as hirudotherapy and ichthyotherapy are used. Such methods cannot be considered traditional, and many doctors are skeptical about them. However, if treatment with leeches can cause adverse reactions, then treatment with fish is a painless natural stimulator of skin microcirculation.
The stationary stage also involves taking a vitamin complex, taking antihistamines and following a diet. In addition, the doctor can prescribe additional methods of therapy on an individual basis, based on the overall picture of the disease.
How to treat psoriasis?
Treatment of the disease must be carried out by a qualified doctor and individually for each patient. Treatment depends on the patient’s age, general health, profession (the influence of occupational factors), gender and personal characteristics of the patient. The nature of the course of the disease and its stage are established, and provoking factors are eliminated (drinking alcohol, drug intolerance, allergic diseases).
Attention is paid to the general condition of the patient (psychological and physical). Normalization of the environment, rest, short hospitalization or change in work schedule can make changes in the course of the disease. If signs of psoriasis are detected, it is recommended to immediately seek medical help. It is the doctor who prescribes various drugs and other therapeutic methods.
One of the newest and most effective methods of treating psoriasis is genetically engineered biological drugs (GEBP), the second common name is biology.
The principle of action of these drugs is to act on various molecules that cause inflammation and contribute to the formation of plaques, damage to nails, and joints. The first GEBDs acted on the tumor necrosis factor, reduced the manifestations of psoriasis, but at the same time weakened the body's anti-infective (especially anti-tuberculosis) and anti-tumor immunity. Modern drugs block IL-17, which is responsible for the appearance of psoriatic plaques. The effect on interleukin IL-17a is targeted and only slightly affects the normal functioning of the body’s immune system. Such drugs are well tolerated by patients.
How to use genetically engineered biological drugs? GIBPs were developed quite recently, less than two decades have passed since their appearance. Unfortunately, psoriasis cannot be cured completely, but with the help of long-term constant use of biologically active drugs it can be brought into long-term remission. This is exactly the option when a person with psoriasis can lead a normal life without the presence of manifestations of the disease.
Treatment begins with several frequent injections (induction therapy), then only maintenance injections are required once at a certain period of time.
Often, an obstacle to the treatment of psoriasis with biologically active drugs is their high price. But now there are drugs available at affordable prices for independent purchase.
Therapeutic therapy can be depicted in the following table:
| Systemic therapy (indicated for severe cases or lack of effect from local treatment) | Local treatment (indicated in all cases of psoriasis alone or in combination with other methods) | Instrumental methods (Assigned differentiated and individually) |
|
|
|
On the subject: Treatment of psoriasis - a review of effective remedies
Essential minerals and vitamins for psoriasis
Silicon for psoriasis. In recent years, the issue of silicon deficiency as one of the causative mechanisms of psoriasis has been increasingly discussed. Therefore, it is advisable to include drugs based on it in the treatment complex at any stage of the disease. The mechanism of their action is in two directions. On the one hand, silicon, after absorption in the intestine, is transported to the affected skin, improving its structure, on the other hand, it acts as a sorbent, absorbing all antigenic complexes from the systemic bloodstream and removing them with feces.
Vitamin D for psoriasis. An extremely important trace element for the successful fight against psoriasis is calcium. But it is practically not absorbed without vitamin D. Therefore, preparations based on it are necessarily included in the treatment process. It is best to take them after the active phase of the disease has been transferred to stationary or remission. The role of calcium and vitamin D is that they stabilize cell membranes, reducing the release of inflammatory mediators into the blood. Before taking specific products, it is better to familiarize yourself with their composition, since most of them contain both of these components.
Fish oil for psoriasis. Any inflammation is accompanied by severe acidification of the environment and cell death. To better restore them and bring the immune system into balance, antioxidants are needed. Omega-3 acids found in fish oil are among the most powerful. Therefore, it is highly desirable to include them in the complex of treatment measures for psoriasis.
Lecithin for psoriasis. The result of psoriatic inflammation is massive death of epithelial cells. For their rapid restoration, phospholipids are needed, which act as the basic building material of all body tissues. One of the most powerful sources of these compounds is lecithin. By including drugs based on this substance, you can achieve faster relief of inflammatory manifestations and restoration of the skin (
Treatment methods
Therapy will necessarily be systemic and complex, consisting of several types of medications for internal and external use. The treatment methods used can be divided into several categories.
- Medications. This is a complex of anti-inflammatory, antihistamine, detoxifying agents. They are used externally and internally. Practice shows that external medications work better, but to help them with widespread lichen planus, doctors prescribe injections, droppers and tablets. Diclofenac, Methotrexate, Acitretin, etc. are actively used.
- Vitamin complexes. A separate group of drugs whose action is aimed at raising and restoring the immune system. With their help, the condition of the skin improves and a protective barrier against infections is created. The doctor may recommend both vitamin complexes in the form of tablets, or simply focus on eating different fruits, vegetables and foods high in essential vitamins and microelements.
- Physiotherapeutic procedures. Chemophototherapy, based on the use of photosensitizing drugs and long ultraviolet waves, is considered the most effective and useful. Complex exposure helps to enhance the impact of radiation and minimize potential damage. With the help of physiotherapy, it is possible to stabilize metabolic processes, stop cell growth, and help restore the skin. Based on a specific situation, procedures can be carried out several times a week for 1 – 2 months. But chemo-phototherapy is recommended in the most difficult cases of widespread psoriasis. For easier stages, selective methods of ultraviolet exposure without the use of a drug are used.
- Methods of traditional therapy. Here the opinions of dermatologists differ. Some actively support the use of traditional medicine, while others are against it. But since pharmacology has not been able to develop effective remedies against psoriasis, a number of patients prefer cheaper and safer folk recipes. Plus, it cannot be denied that the recipes of many medicinal ointments, creams, gels and other products sold in pharmacies are based on folk remedies. Consider the likelihood of an allergic reaction and individual intolerance. The attending physician must be aware of what you are using during treatment in parallel with the prescribed drugs.
- Homeopathy. An even more controversial method of influencing lichen planus vulgaris than traditional medicine. But there are a number of homeopathic remedies that medicine recognizes. Many doctors and entire sanatoriums base therapy against dermatological diseases on homeopathy. Consult your doctor before using such products.
- Surgical intervention. It is used extremely rarely and only in cases where psoriasis affects the joints. And then this happens in exceptional situations. Only a doctor can decide on surgical intervention if there is a threat to life or the risk of completely losing the mobility of certain joints.
- Prevention. Since psoriasis is a chronic pathology, prevention is included in the list of methods of its treatment. Here, patients should rely on maintaining a healthy lifestyle, proper nutrition, timely treatment of infectious diseases, protection from stress and other tips.
Competent treatment tactics and compliance with the rules of prevention will not help to completely recover from scaly lichen. But such measures can ensure stable and long-term remission. There are many examples of people coping with widespread psoriasis and preventing it from recurring for many years.
Be healthy and do not forget to periodically undergo examinations and tests for prevention. This allows you to prevent diseases and maintain the body in excellent condition.
Subscribe, leave your comments and tell your friends about us!
Prevention
The main preventive measure for limited psoriasis is considered to be a healthy diet and a healthy lifestyle.
It is worth noting that this rule applies not only to relapses, but also to remissions. Periodically, you need to cleanse the body of accumulated toxins in order to eliminate overload of the skin. It is imperative to monitor the condition of the intestines, avoiding constipation and diarrhea.
You need to be especially careful when taking medications that are intended to combat other ailments.
In addition, you should cook food using sea salt, and also take relaxing baths with this trace element. The use of flaxseed oil, nettle and brewer's yeast will be beneficial.
It is also worth considering that if psoriasis recurs, you need to give up foods that contain milk and gluten.
Principles of treatment
Only an experienced specialist can prescribe effective therapy, since each case is individual. The patient’s age, gender, the influence of negative professional factors, as well as general health status must be taken into account.
Most often, localized psoriasis is treated with topical medications, diet, and quality physical therapy. In some cases, patients prefer to use folk remedies.
Ichthyol ointment accelerates tissue regeneration
Experts say that emollient creams (Ichthyol, tar) show good results. Herbal remedies - Colhamin ointment, as well as Psoriaten.
In some cases, laser therapy, ultraviolet irradiation of inflammatory foci, extracorporeal blood purification, and selective phototherapy may be used.
Symptoms and signs
When a patient develops lichen planus, he is faced with the following symptoms:
- after removing the plaques, a smooth and moist film appears on the skin;
- suppuration occurs in the cracks formed in the affected areas;
- certain areas of the skin are covered with light-colored plaques;
- drops of blood form under the scales;
- severe itching;
- irritability;
- prostration.