Causes
Xanthomatosis is usually caused by high levels of lipids, that is, fats, in the blood. Also, xanthomas on the skin appear in diseases accompanied by lipid metabolism disorders:
- atherosclerosis;
- diabetes;
- hypothyroidism;
- primary biliary cirrhosis of the liver;
- cholelithiasis and other types of cholestasis;
- nephrotic syndrome in kidney disease;
- hematological diseases;
- malignant tumors;
- side effect of taking prednisolone, tamoxifen or cyclosporine.
One of the reasons for the appearance of xanthoma on the skin in young people is familial hyperlipidemia, accompanied by an increase in the level of triglycerides and cholesterol in the blood.
Xanthomas themselves are not dangerous. However, it is necessary to identify their cause. First of all, you need a consultation with a dermatologist and an examination by a therapist. If necessary, the patient continues treatment with a cardiologist, endocrinologist, nephrologist, hepatologist, hematologist, or oncologist.
Prevention and recommendations
Prevention of xanthoma is carried out only with the awareness that the patient suffers from hyperlipemia or other primary diseases. Recommended:
- maintain normal weight;
- practice regular physical activity, especially aerobics;
- follow a proper diet, limiting the consumption of foods that are not recommended for consumption with high cholesterol, increasing the amount of foods that are useful for reducing high cholesterol;
- use medication prescribed by your doctor.
Symptoms
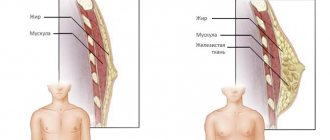
Xanthomas on the skin associated with the accumulation of fats are clinically divided into several options:
- flat;
- intertriginous;
- palmar;
- tendon;
- tuberose;
- flat eruptive.
Sometimes there is a combination of several types.
Flat
The most common type of formation. Xanthomas are asymptomatic and appear on the skin as soft, velvety, flat, polygonal yellow elements. Most often, a flat xanthoma of the eyelids is observed, at the inner corner of the eye. Sometimes they reach gigantic sizes.
Tuberous (lumpy)
These are firm, painless, red-yellow nodules. Lesions on the skin can be multiple and merging. Such xanthomas usually develop in places of friction and pressure, for example, on the extensor surfaces of the knees, elbows, and buttocks. Sometimes they appear on the skin of the cheeks or the bridge of the nose.
Tendon
Slowly enlarging subcutaneous nodules associated with tendon and ligament tissue. These include gouty tophi, affecting the big toe. Such xanthomas most often occur in the extensor area of the upper limbs and in the Achilles tendon.
Eruptive
Eruptive xanthomas on the skin are localized mainly on the buttocks, shoulders, and extensor surfaces of the limbs. Sometimes the mucous membrane of the mouth and face are affected. The lesions are rashes of red-yellow papules on reddened skin. They are accompanied by itching and sensitivity to the touch.
Xanthomas on the palms look like spots; they can appear on other parts of the body. The palmar fold is most often affected by type 3 dyslipoproteinemia.
In patients with normal blood lipid levels, special disseminated and verrucous forms of xanthomatosis occur.
1. Tendon xanthoma 2. Eruptive xanthoma
Disseminated form
The disseminated form of xanthomatosis is observed mainly in adults and looks like multiple red-yellow tubercles and nodules located in the folds of the skin, as well as numerous xanthelasmas on the eyelids. In diffuse xanthomatosis, the skin is affected in the form of yellow plaques under the eyes, on the neck, upper torso, buttocks and in skin folds. In rare cases, the oral cavity is additionally involved.
Verrucous form
Such xanthomas occur primarily in the oral cavity of adults. These are single asymptomatic lesions. They can also be localized on the forearms, limbs, anogenital area, as well as on the walls of the esophagus, making swallowing difficult.
Xanthelasma
A type of xanthoma. Xanthoma is similar in appearance to a yellow subcutaneous formation that appears on the limbs, buttocks and other areas of the skin, and xanthelasma rises above the skin surface, forming a tumor-like formation, primarily around the eyes.
Clinical manifestations
The typical location of plaques is the face, but the torso, feet, palms, and natural folds of the skin are also often affected. Symptoms are individual for each patient.
Clinical characteristics of formations:
- The color of the plaques varies from light yellow to dark brown. Dark xanthomas are often mistaken for melanomas.
- Xanthomas may be flat or raised above the surface of the skin.
- The dimensions usually do not exceed 10 millimeters. In rare cases, the dimensions reach several tens of centimeters.
- The surrounding tissue is dry and flaky. This indicates trophic disorders of the skin.
- Formations are characterized by slow but progressive development.
- Cholesterol plaques on the skin never degenerate into cancer.
Complications of xanthomatosis
Typically, xanthomas on the skin do not cause any complications. Health problems can arise if you do not pay attention to the causes of this condition. In this case, the likelihood of hypertensive crises, angina pectoris and myocardial infarction, ischemic stroke and even death increases.
As a rule, most xanthomas on the eyelids do not affect vision. However, there is a small chance that a large formation will cause ptosis - drooping eyelid. As a result, vision in the affected eye gradually deteriorates.
Large xanthomas on the skin can change the patient's appearance, causing cosmetic defects.
Associated conditions
The presence of skin xanthoma in a patient may indicate the possibility of the following diseases and conditions:
- myocardial infarction, aortic valve pathology, as well as pancreatitis;
- large single flat elements sometimes accompany chronic myelomonocytic leukemia, mastocytoma, and ultraviolet ray damage;
- POEMS syndrome (polyneuropathy, organomegaly, pathology of the endocrine glands, skin changes caused by M protein), systemic sarcoidosis and insufficient number of liver bile ducts;
- primary or secondary hyperlipidemia - an increase in fat content in the blood caused by hereditary diseases or atherosclerosis.
Disseminated xanthomatosis affects various internal organs, and patients experience difficulty swallowing, shortness of breath, and blurred vision. The functioning of the central nervous system and musculoskeletal system is disrupted. Such xanthomatosis is often associated with lymphoproliferative diseases and hematological malignancies, such as leukemia. In addition, these patients have an increased likelihood of oral candidiasis, Budd-Chiari syndrome, rheumatoid arthritis, and Hand-Schuler-Christian disease.
The verrucous form of xanthomatosis accompanies the following diseases:
- lichen planus;
- Paget's disease;
- epidermal nevus;
- discoid lupus erythematosus;
- pemphigus vulgaris;
- dystrophic epidermolysis bullosa;
- chronic graft-versus-host disease;
- actinic keratosis;
- squamous cell carcinoma;
- congenital developmental defects;
- consequences of PUVA therapy with psoralen or radiation treatment;
- period after bone marrow transplantation.
Common xanthoma
- Xanthoma-like lesions are caused by a rare form of histiocytosis.
- Lipid metabolism is normal.
- The skin lesions usually consist of hundreds of small yellowish-brown or reddish-brown bumps that are usually evenly distributed on both sides of the face and torso. They can be especially hard on the armpits and groin.
- Small bumps may join together to form sheets of thickened skin.
- In 30% of affected people, the mucous membranes of the mouth, respiratory tract or eyes (mucous membranes) are affected. Warty plaques in the mouth are called verruciform xanthoma.
- 40% of affected people develop diabetes insipidus, a condition that results in an inability to control water loss (leading to constant thirst and excessive urine production). This occurs due to the overgrowth of histiocytes on the lining of the brain (meninges).
- May affect internal organs (eg liver, lungs, kidneys, etc.)
- Self-limiting and eventually improves on its own, but may persist for many years.
Diagnosis of xanthomatosis
The doctor studies the state of lipid metabolism to identify primary and secondary hyperlipidemia. Blood tests are used for cholesterol, low- and high-density lipoproteins, and triglycerides. Liver and kidney function tests are performed.
To confirm xanthomatosis of the Achilles tendon, ultrasound and MRI are used. For disseminated xanthomatosis, positron emission computed tomography can be used to identify the severity of the disease and assess the effectiveness of treatment.
In doubtful cases, a histological examination of tissue obtained from these formations is prescribed. In this case, vacuolated or foamy macrophages are determined - cells that have absorbed fat, which dissolved during processing of the biopsy sample.
Eruptive foci may contain inflammatory infiltrates; verrucous, tendinous and tuberous - connective tissue.
Wide range of results
Polygenic familial combined hyperlipidemia: type IIb
- Mixed genetic and life history causes
- Elevated total cholesterol levels
- Elevated triglyceride levels
- Low HDL (High Density Lipoprotein) Cholesterol
- Elevated LDL cholesterol levels
- LDL may be normal levels but denser and more likely to cause atheroma (sebaceous cyst)
Moderate hypertriglyceridemia
- Often also associated with high blood pressure, obesity, diabetes, metabolic syndrome, high insulin levels, high uric acid levels
- This may be due to alcohol or medications such as systemic steroids, isotretinoin, acitretin
- Triglycerides 2_10 mmol/l
- Often associated with low HDL cholesterol levels
Severe hypertriglyceridemia: Types 1 and V
- Mixed genetic and life history causes
- Diabetes
- Familial LPL (lipoprotein lipase) deficiency
- Triglycerides > 10 mmol/l
- Elevated total cholesterol levels
- Raised chylomicrons
- Elevated LDL cholesterol levels
Wide beta hyperlipoproteinemia: type III
- Rare mutation of the apo E gene
- Triglycerides 5-20 mmol/l
- Total cholesterol 7-12 mmol/l
The reason for the appearance of xanthoma with normal levels of fat in the blood is currently unclear.
Treatment of xanthomatosis
Eruptive xanthomatosis
Is it possible to remove xanthoma and how to do it
Xanthomatosis is treated with medications or surgery.
Xanthomas are not always associated with hyperlipidemia, but if it is present, it requires mandatory treatment. This will not only reduce the risk of complications of atherosclerosis, but also reduce the size of the pathological formation itself. In severe hypertriglyceridemia, the main goal of treatment is the prevention of pancreatitis.
To treat hyperlipidemia, a special diet and lipid-lowering drugs are used. The latter include statins, fibrates, bile acids, resins, probucol and niacin. After starting to take them, eruptive xanthomas begin to disappear within a week, tuberous xanthomas after a few months, and tendinous xanthomas within several years.
The formation itself can be removed using trichloroacetic acid applications.
If drug therapy is ineffective or inappropriate, xanthomatosis is treated surgically, but lipid-lowering drugs are still not canceled to reduce the risk of systemic complications of hyperlipidemia.
Removing xanthomas using excision with a scalpel is a very effective, but also the most traumatic method. During surgery, bleeding inevitably occurs and there is a risk of infection. After the intervention, almost all patients are left with small scars.
Usually the formation is removed with a laser, excision followed by skin grafting, removal using cryodestruction or electrocoagulation.
Laser technique is the most popular for the treatment of xanthomatosis. Its effectiveness largely depends on the skill of the surgeon. An experienced doctor can remove all lesions in one session without damaging the dermis and thereby minimizing the risk of scarring. The operation is performed under local anesthesia, the patient's eyes are protected with special glasses.
Electrocoagulation (cauterization using high temperature) has the following advantages:
- lower cost than laser removal;
- no risk of retinal burns.
Cryotherapy is rarely used to eliminate xanthelasmas. This is due to the difficulty of protecting the eyes from the effects of low temperatures, as well as the greater likelihood of scarring compared to other methods. However, the advantage of such an intervention is the extremely low risk of infectious complications.
After surgery, relapses of xanthomatosis and complications are possible, for example:
- temporary redness of the skin;
- infectious complications, suppuration;
- scarring;
- formation of dark spots - hyperpigmentation.
With disseminated xanthomatosis, various internal organs may be involved in the process, which determines the severity of the disease. In other cases, the disease has a benign course. In some cases, xanthomas may disappear spontaneously. They never turn into skin cancer.