Definition
Ripping after mammoplasty is a complication characterized by the formation of small folds, “waves” or “ripples” on the breast.
It represents a visual manifestation of the implant.
When the implant is positioned vertically, its upper part rolls into the lower part, and folds form at the top (typical of saline implants). When the skin is over-tensioned, these folds begin to appear.
Ripping may not appear when the glands are in a quiet position and can only be detected when the body is tilted or while walking.
A defect can occur due to the physiological characteristics of the body, insufficient volume of skin, incorrectly selected implants, violation of surgical technique, etc.
The likelihood of ripping directly depends on the size of the selected implants. The larger they are, the sooner a defect will occur.
Causes
Seroma after mammoplasty is considered a complication not so much dangerous as unpleasant.
Main causes:
- During the operation, the lymphatic vessels were affected - vascular restoration is observed already in the first day after surgery, but in some cases the process occurs much more slowly, which leads to the accumulation of lymph.
- Negative reaction to suture threads - even a wide range of modern threads for sutures cannot guarantee that the body does not have a negative reaction to a foreign object. Excessive use of suture material also poses a risk of complications.
- Tissue bleeding appears - small capillaries may well penetrate into the gland tissue and settle at the site of the implant, causing the accumulation of lymph.
- The drainage procedure is poorly carried out - a drainage system is used to remove excess fluid during any operation. If the procedure was carried out incorrectly, then perhaps the cause of seroma lies precisely in this.
- Rejection of the prosthesis - modern biomaterials used for the manufacture of implants, in most cases, take root normally in the human body. However, there is still a slight chance of rejection. At the moment, scientists have not been able to develop a system for detecting negative reactions to the implant before surgery.
- The appearance of a hematoma on the chest - if a hematoma forms after surgery, it is necessary to regularly consult with the attending physician, since tissue healing can lead to the accumulation of blood substances and the beginning of the development of seroma.
Women who have had a mastectomy have the greatest risk of developing seroma after surgery due to the active development of the lymph nodes. Factors that increase the risk of its occurrence include: diabetes, obesity, old age, and high blood pressure.
Why does it appear
Often, a similar effect appears after surgery, when the swelling subsides, but the skin still remains stretched, poorly contracted and gathers in folds. In this case, implants have nothing to do with it; this is a temporary phenomenon.
There are several factors that influence the risk of this complication:
- volume and elasticity of the skin and soft tissues;
- type and size of implant;
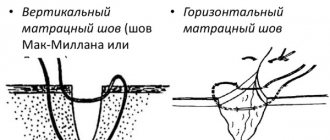
- place and technique of administration.
“Waves” most likely will not appear or will be barely noticeable if the volume of the skin is sufficient to properly cover the implant.
This is why ripping appears more often in petite women with a thin layer of fat and small mammary glands.
In obese patients with a pronounced layer of subcutaneous fat and initially voluminous breasts, this problem, on the contrary, does not exist.
In general, it is believed that the more implants are selected, the higher the risk of ripping.
The location of the prosthesis plays an important role. Submuscular placement of the implant (i.e., under the muscle) is preferable.
Thanks to this, a larger volume of soft tissue is formed over the prosthesis, and the muscles themselves have their own tone, which also helps hide the defect.
Since the muscle only covers half or 2/3 of the top of the implant, it is still possible for ripples to form in the area of the lower gland fold.
Photo: Ripling
But this place itself is hardly noticeable, and even with deep probing you can feel something, but not see anything special. That is why a little ripping is perceived quite normally here.
The pectoral muscles are usually well developed in the center and become thinner and flatter towards the outer border of the rib cage.
Therefore, when the prosthesis is inserted under the muscle, the outer edge of the tissue volume may not be enough, and ripples from the side become noticeable (especially when bending). If such a defect is unacceptable, you will have to opt for smaller implants.
Ideally, the width of the prosthesis should be less than the diameter of the mammary glands before mammoplasty.
The “washboard effect” often occurs when placing saline implants that are filled with saline solution.
In addition, in addition to the waves along the edges of the prosthesis, where there is a lack of native tissue, such implants give the effect of ripples over the entire surface of the gland.
This is the result of free movement of fluid inside the prosthesis when it is not filled enough. Ripping is especially pronounced when the implant is placed over the pectoral muscle.
Gel implants do not have this drawback, which is why most clinics now use them.
Regarding the surface, rough implants, compared to smooth ones, increase the risk of ripples.
This is due to the fact that your own tissues seem to “stick” to the textured surface.
But this point is relevant only when installing the prosthesis over the pectoral muscle, and not when inserting it subpectorally.
Treatment of seroma after mammoplasty
In most cases, seroma resolves on its own within a few days, less often it accumulates, causing physical discomfort to the patient and leading to more serious complications. That is why regular examinations after mammoplasty are very important; this will promptly prevent the risk of complications, and in cases of complications, quickly eliminate them.
Treatment of seroma after mammoplasty includes:
- medicinal method - treatment with antibiotics and anti-inflammatory drugs, helps in cases of small amounts of accumulation of serous fluid;
- surgical method - installation of drainage through small punctures, as a rule, drainage is installed for several days to drain excess fluid and blood;
- combination of drug and surgical treatment;
- vacuum aspiration – a special device uses a vacuum to pump out fluids from tissues through newly dissected postoperative scars.
Lack of treatment can lead to serious problems - suppuration, necrosis and capsular contracture. In this case, treatment will consist of removing the implants. Remember, timely examinations, strict adherence to the rehabilitation period, and most importantly, a competent choice of surgeon - guarantee a successful outcome of the operation and minimize the risk of seroma after mammoplasty.
© PlasticRussia, 2020. All rights reserved. Full or partial copying of site materials without the consent of the portal administration is prohibited.
2
What does ripping look like after mammoplasty?
Ripping looks as if your fingers ran across the iron and small “grooves” were left on the surface.
With a small amount of tissue, wrinkled breasts do not look particularly aesthetically pleasing.
The washboard effect is not a fixed defect. This means that it is usually invisible, but can be visualized while walking or bending over.
The ripples can be small and unnoticeable to others and can only be felt when running your hand over the skin.
Some women don't mind ripping at all if they find it acceptable. But for others, the defect becomes a real problem, which can only be solved surgically.
Photo: Implant shrinkage
Where is it formed
If the implant is inserted under the pectoral muscle, waves will most likely appear at the edges of the chest, since there are no muscles there to cover the prosthesis.
As you lean forward, the ripples become more noticeable as they pull on the skin.
Ripping occurs more often with the introduction of saline implants, especially if there is little natural fatty tissue in the mammary glands.
This effect is explained by the chemical properties of the water-salt solution that fills the prosthesis.
When placing gel implants, ripping is rarely a concern, since the viscous gel holds its shape well.
If implants are too large, the bust may take on a rectangular shape instead of a beautiful smooth outline. And in the area where the muscles cannot cover the prosthesis, pronounced skin wrinkling will occur.
Read when you will have your first period after mammoplasty.
What should breast care be like after mammoplasty? Details here.
What to do
There are ways to eliminate the problem, but they are all surgical. Therefore, it is better to try to avoid a defect during the initial consultation and surgery by choosing suitable implants and the method of their insertion.
Previously, ripping was eliminated by replacing saline implants with gel ones or by moving them under the mammary gland if they were installed above it (under the mammary glands).
Now, several solutions are available to solve this problem.
Implants can be replaced with high-density gel prostheses; they can be installed under the chest muscles; a dermal matrix can be introduced into the area where this complication is formed, which will hide the waves.
In some cases, the defect can be eliminated by introducing your own fat layer into the problem area.
If ripping is caused by the installation of a saline implant or its insertion above the pectoral muscle, the best solution is to repeat the operation and replace the saline prosthesis with a gel one (in the first case) and installing an implant under the muscle (in the second).
If the skin itself is thin and there is not enough gland volume, you can pay attention to the introduction of a dermal matrix (Alloderm). This technique will help reduce wrinkles.
Alternatively, you can transplant fat tissue, which will give your own tissues additional volume.
Another solution to the problem is to replace the prosthesis with a smaller one. But if you absolutely don’t want to change the size, it’s better to just leave everything as it is and not pay attention to the defect.
Complications arising from the appearance of a postoperative fistula
- – a cavity filled with pus;
– inclusion of subcutaneous fat in the inflammatory process;
Eventration – loss of internal organs due to purulent melting of tissues;
– spread of purulent contents in the cavity of the chest, skull, and abdominal cavity;
Toxic-resorptive fever is pronounced hyperthermia as a reaction of the body.
Found an error in the text? Select it and a few more words, press Ctrl + Enter
The primary diagnosis of a ligature fistula is carried out in the dressing room during a visual examination of the wound by a surgeon. To clarify the location of the fistula, the presence or absence of complications (abscess, purulent leaks), an ultrasound scan of the surgical wound is performed.
If the fistula is located deep in the tissue and its diagnosis is difficult, fistulography is used. During the examination, a contrast agent is injected into the fistula tract and radiography is performed. As a result of such manipulation, the fistula tract will be clearly visible on the x-ray.
The vast majority of cases of ligature fistula can only be resolved through surgery. The longer a postoperative fistula exists, the more difficult it is to cure. Complex therapy using medications is used for treatment.
Groups of drugs used to treat fistula:
- Local antiseptics - water-soluble ointments (Levosin, Levomekol, Trimistan), fine powders (Gentaxan, Tyrozur, Baneocin);
Antibacterial agents – Ampicillin, Norfloxacin, Ceftriaxone, Levofloxacin;
Enzymes for the destruction of dead tissue - Trypsin, Chymotrypsin.
Since the drugs retain their effect for several hours, they are injected into the fistula tract and distributed throughout the tissues surrounding the wound several times a day.
Fat-based ointments (Synthomycin ointment, Vishnevsky ointment) prevent the outflow of pus, so they are not used in the presence of extensive purulent discharge.
In addition to surgical and drug treatment, physiotherapy is used:
- quartzization of the wound surface;
UHF therapy.
As a result of the use of UHF therapy, microcirculation of blood and lymph improves, which leads to a decrease in swelling and stops the spread of infection. Quartz treatment has a detrimental effect on pathogenic bacteria, promoting stable remission of the process, although not guaranteeing complete recovery.
The “gold standard” for treating a ligature fistula is an operation that eliminates the problem completely.
Progress of the operation to eliminate the ligature fistula:
- Three-time treatment of the surgical field with an antiseptic in the form of an alcohol solution of iodine.
Injection of an anesthetic solution into the tissue around the surgical wound and under it (Lidocaine - 2% solution, Novocaine - 5% solution).
Injection of dye into the fistula tract in order to completely examine it (“green paint” and hydrogen peroxide).
Dissection of the fistula, removal of the ligature completely.
Removal of the cause of the fistula along with revision of the surrounding tissues.
Stop possible bleeding with an electrocoagulator or hydrogen peroxide 3%, since suturing a blood vessel can provoke the appearance of a new fistula.
Wash the wound with antiseptics (Dekasan, 70% alcohol, Chlorhexidine).
Closing the wound with sutures again with the installation of active drainage.
After the operation, the patient needs dressings and drainage rinsing. If the purulent discharge is not fixed, the drainage is removed.
Medicines used in the presence of complications (phlegmonous inflammation of the tissue, purulent leaks):
- Antibacterial agents;
Non-steroidal anti-inflammatory drugs (NSAIDs) – nimesil, diclofenac, dikloberl;
Ointments for tissue regeneration - troxevasin and methyluracil ointment;
Herbal preparations with vitamin E (aloe, sea buckthorn oil).
Local revision of inflamed tissues with wide dissection of the fistula is a classic form of surgical treatment of postoperative fistula. Most minimally invasive techniques are ineffective in treating this complication.
Self-medication of a ligature scar will not bring recovery, because only surgery and subsequent debridement of the wound can save the patient from complications. When attempting self-treatment, precious time will be lost.
Risks and complications
In general, it is believed that ripping is not a classic surgical complication.
However, focusing on the possible dissatisfaction of patients, plastic surgeons try, whenever possible, to make any attempts to minimize the possibility of skin ripples.
This is more an aesthetic problem than a medical one, so, as a rule, there is no talk of serious risks and complications.
Not every patient is ready for a second operation, so most often everything is left as is.
Ripping can hardly be called a complication, since waves do not always appear, but only when the body bends forward or during active movements. It may be visually faintly noticeable, and only the woman herself can feel the unevenness.
Find out why breast pain occurs after mammoplasty.
Do scars appear after mammoplasty? Read more.
How long after mammoplasty can I play sports? Details here.